Breast Implant Complications
Breast augmentation is a common plastic surgery procedure, with women getting breast implants for various reasons. Breast implants can cause a significant health risk despite numerous years of advancement.
Patients undergoing breast augmentation surgery may experience different complications throughout the journey. This may be after a short while or years later after the surgery.
Most complications are rare, and many women may not experience them at any point. However, it’s essential for all women considering undergoing breast augmentation to be aware of the complications. Learn more about breast augmentation, implant-related complications, and everything involved from this comprehensive article.
Top Reasons for Breast Augmentation
Breast augmentation is a plastic surgery procedure carried out in women to enhance the size and shape of the breast. Breast augmentation is mainly classified as cosmetic or reconstructive surgery.
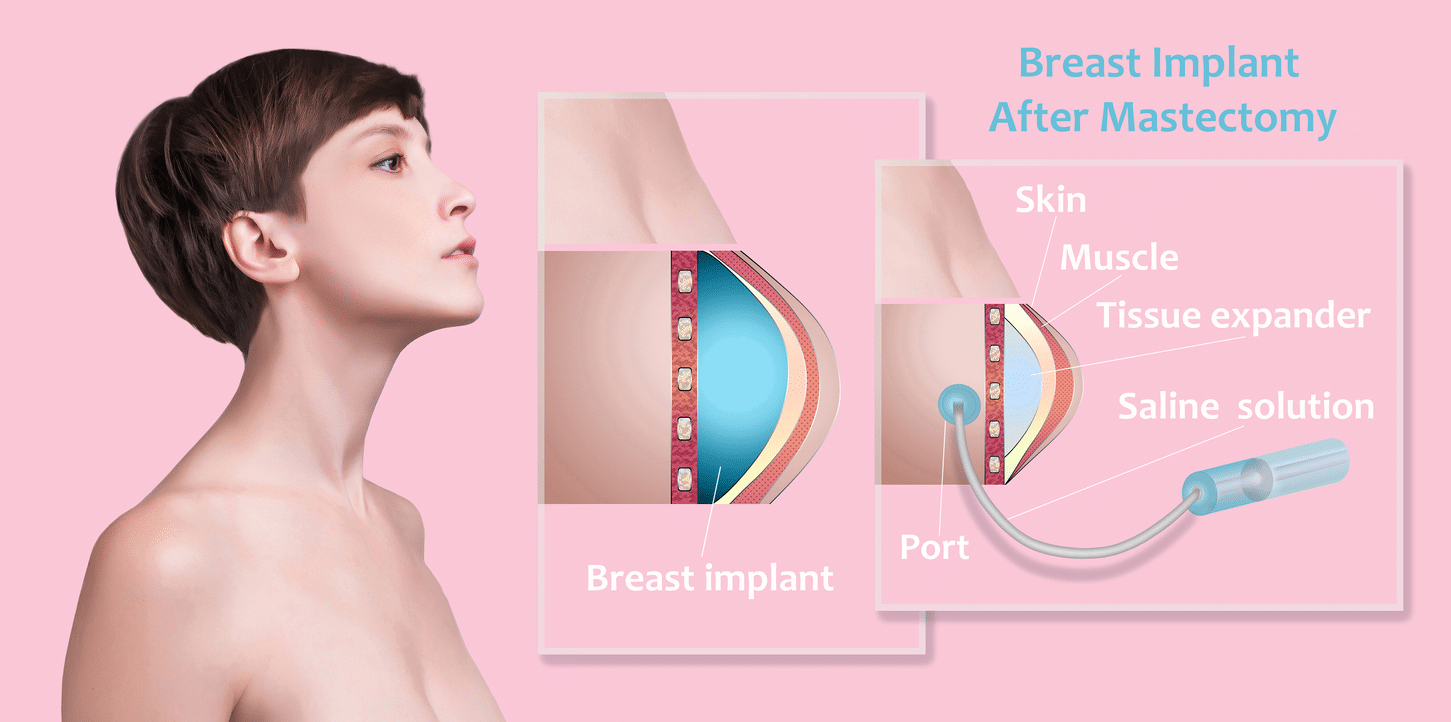
Cosmetic surgery involves breast surgery to enhance the body’s appearance. On the other hand, reconstructive surgery is carried out mainly for medical reasons, most commonly after breast cancer surgery. Reconstructive surgeries are deemed medically necessary, meaning the patient needs the surgery for the body’s normal functioning.
Different types of breast implants are used for breast augmentation. The choice depends on several factors, including body type, implant size, shape, texture, and more. But what are some of the reasons why women undergo breast augmentation?
- To enhance the breast size and shape.
- To correct unevenness where the breasts vary in size. This may be a pre-occurring condition or caused by a breast implant illness.
- To enhance appearance.
- For breast reconstruction after mastectomy due to breast cancer.
Types of Breast Implants and the Associated Risks
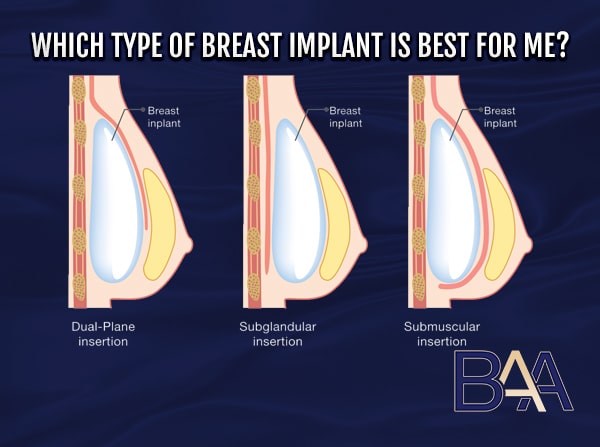
As mentioned earlier, there are different types of breast implants. So, let’s look at them briefly alongside their associated risks. But before that, it is essential to note that breast implants vary in size, shape, and texture. A specialist surgeon will recommend different implants depending on the desired patient’s results. Other factors, such as the type of procedure used, the patient’s anatomy, and cost, may affect the type of implant to use. In addition, different types of implants pose various risks that may lead to complications in the future.
In terms of texture, there are smooth and textured breast implants, while regarding shape, there are round and teardrop implants. Textured implants are either micro-textured or macro-textured. However, the primary classification of breast implants lies in two types, silicone and saline breast implants.
Silicone breast implant
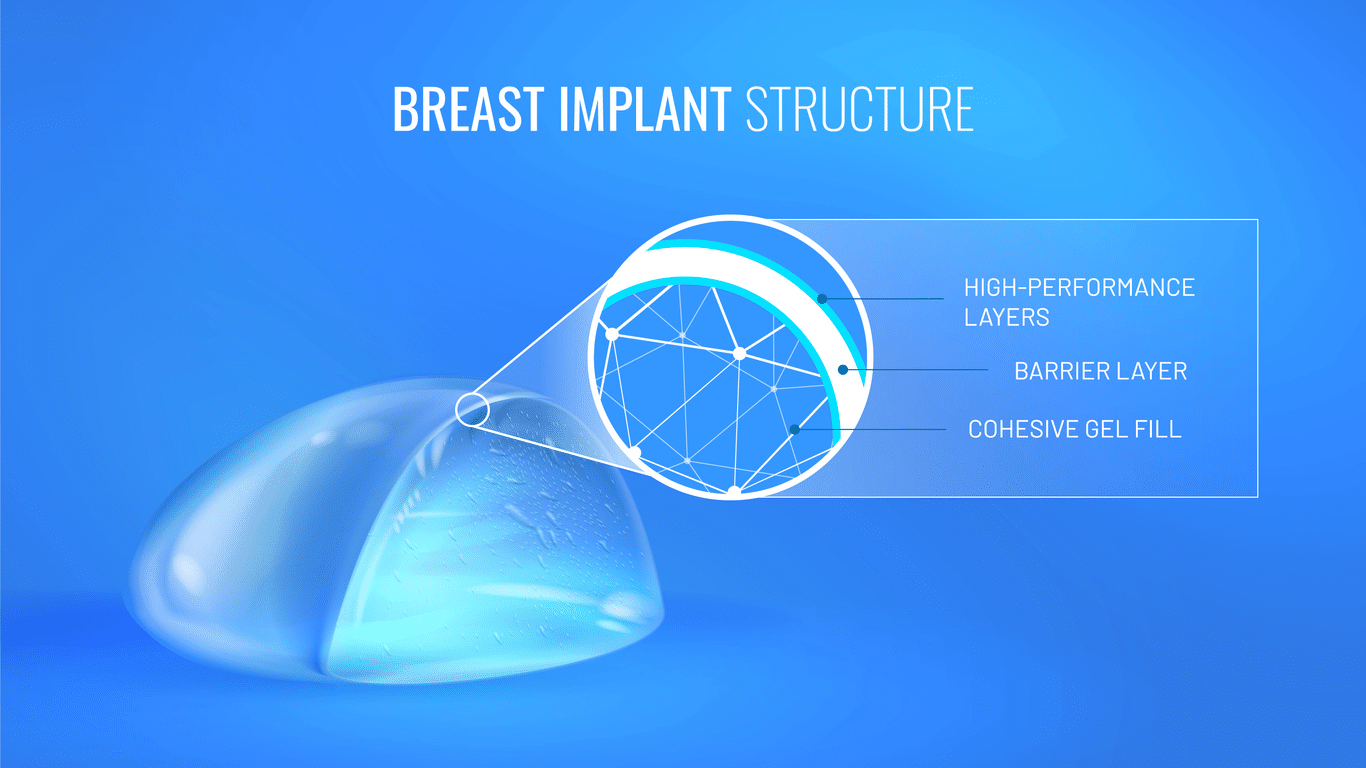
Silicone Breast Implant: These are implants made of a silicone shell and filled with silicone gel. Silicone implants are available in different shapes and can be round or teardrop shaped. In addition, silicone breast implants are either smooth or textured. Silicone implants are used for different purposes, including cosmetic or reconstructive surgery.
The implants are TGA approved for breast reconstructive surgery for women seeking breast augmentation in Newcastle. However, silicone implants are associated with the risk of silent rupture.
Saline Breast Implants: These implants are filled with a sterile saline solution and a silicone outer shell. Like their counterparts, they are available in different sizes and textures. However, unlike silicone implants, saline implants are filled during surgery. Saline implants can be used for cosmetic enhancement or Breast implant reconstruction.
These implants are available for reconstruction in women of any age. However, they also pose a risk of silicone breast implant rupture, folding, and wrinkling, among other implant-related complications.
Common Complications Associated with Breast Implants
Breast implants are associated with various complications. These complications may vary depending on several factors, such as the type of breast implant, the procedure used, and more. Some complications may develop shortly after the procedure, while others develop years later.
In addition, the treatment will vary depending on the complication.
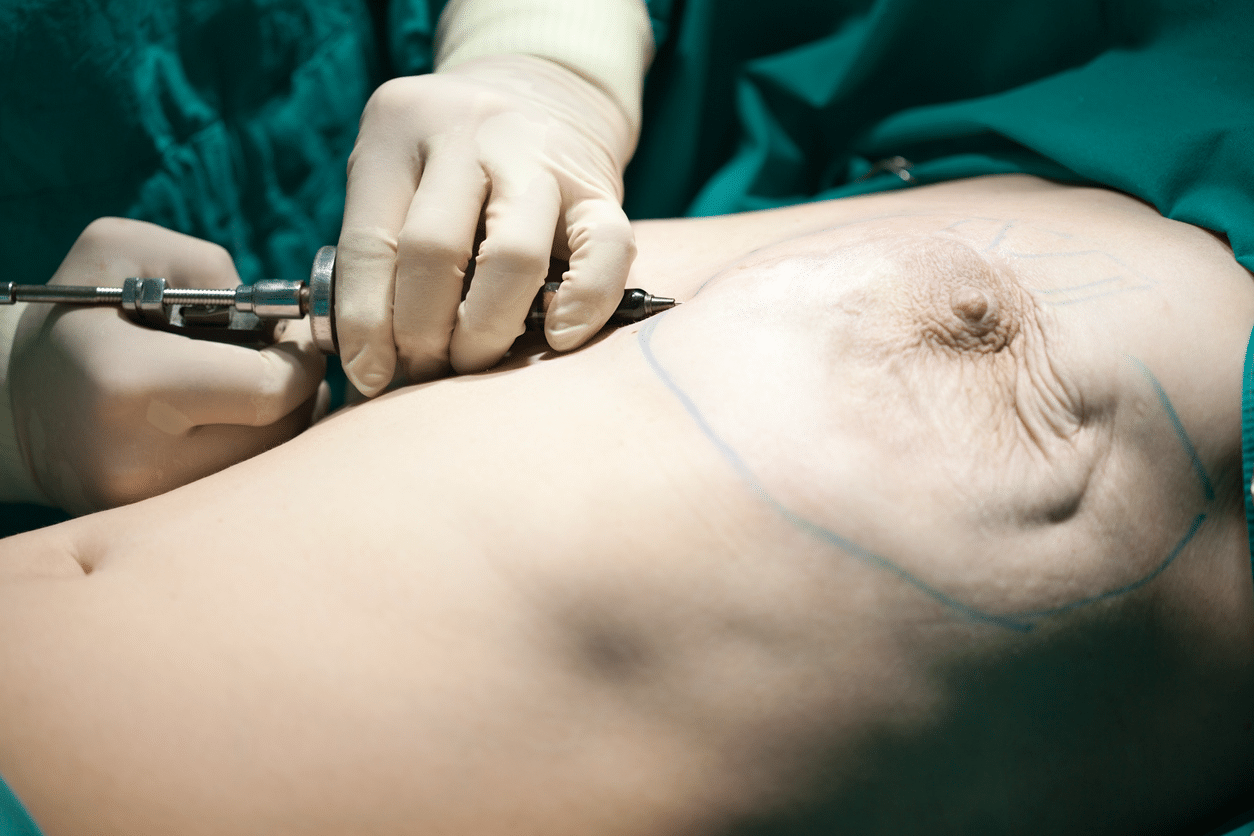
Breast Augmentation Procedure
Capsular Contracture
Capsular Contracture is caused by the hardening of the breast tissue surrounding the implant. After breast surgery, a capsule forms around the implant, keeping the implant in place. However, in some cases, the capsule may harden. The hardening causes tightening of the breast tissue, causing pain and discomfort.
Capsular contracture is commonly associated with seroma, implant texture, rupture, type of incision, and hematoma. However, the leading theory on the cause of capsular contracture is a bacterial infection. The bacterial infection creates a biofilm on the implant surface, affecting the surrounding breast tissue. The bacteria are often due to contact of the implant with foreign material, especially the skin, during insertion.
The condition may occur in only one or both breasts. Capsular contracture mainly occurs within two years after breast augmentation surgery. However, it may occur in some breast implant patients many years after a breast implant surgery.
There is an equal chance of contracting the complication regardless of whether you have silicone or saline breast implants. However, textured implants can reduce the risk of capsular contracture.
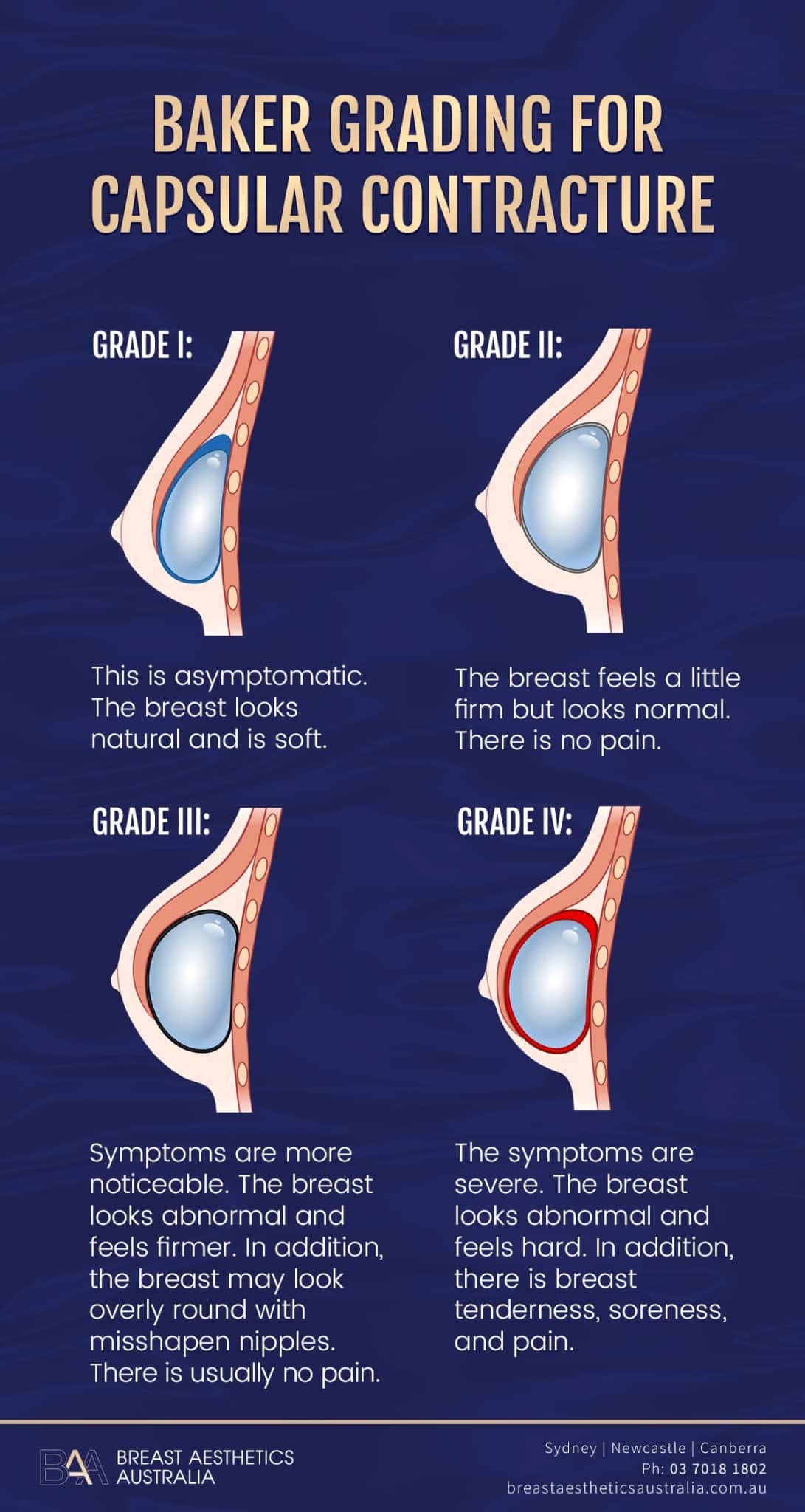
Baker Grading for capsular contracture – Infographic
Doctors use four levels to determine the degree of capsular contracture. The level is determined using Baker Grading.
Grade I: This is asymptomatic. The breast looks natural and is soft
Grade II: The breast feels a little firm but looks normal. There is no pain.
Grade III: Symptoms are more noticeable. The breast looks abnormal and feels firmer. In addition, the breast may look overly round with misshapen nipples. There is usually no pain.
Grade IV: The symptoms are severe. The breast looks abnormal and feels hard. In addition, there is breast tenderness, soreness, and pain.
The last two grades of capsular contracture may require revision surgery for treatment. The revision surgery to treat capsular contracture may involve implant removal with or without implant replacement. However, the revision surgery does not eliminate the reoccurrence of capsular contracture. Most specialist surgeons currently are adopting the use of Keller Funnel to ensure there is less contamination of the breast implant during breast augmentation to prevent capsular contracture.
Ways to Prevent Capsular Contracture
Below are some ways to reduce the risk of capsular contracture after breast surgery.
- Regular patient screening: Women should undergo thorough screening to detect the early stages of complications.
- Using the right implant size: If the surgeon places large implants in a woman with less breast tissue to cover the implant, it may increase the risk of capsular contracture. A patient with insufficient breast tissue should consider increasing breast size in stages, starting with a smaller implant. After allowing the skin to stretch, the patient can consider getting a larger implant. This is why it is essential to schedule a consultation with a specialist general surgeon before the implant surgery to discuss what type, shape, texture etc suits you better.
- Using a no-touch technique during implant insertion: During the insertion process, the surgeon should ensure minimal contact of the implant with the outer material. Therefore, techniques and tools that enhance the no-touch technique should be prioritised. Tools like the Keller Funnel improves the no-touch technique. Some of the methods that enhance the no-touch technique include double-implant loading, reversed-glove sleeve, plastic sleeve, infusion containers, and packaged implant covers.
- Submuscular placement: It involves placing the breast implant under the chest muscle.
- Using textured implants: Textured implants provide a surface for the breast tissue to integrate with the implant. This reduces the implant’s movement, reducing the rate of capsular contracture. However, macro-textured breast implants are banned in Australia due to their association with other complications like BIA-ALCL.
- Breast massage: Massing the breast during the healing may prevent the development of capsular contracture. However, the patient should be cautious not to damage the tissue and should consult a surgeon first.
BIA-ALCL
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) is a cancer associated with breast implants. However, it’s not breast cancer but a rare T-cell lymphoma-immune system cancer. It’s a type of non-Hodgkin’s lymphoma which grows in the scar tissue and fluid around the breast implant.
The most common symptoms of BIA-ALCL include swelling in the breast or around the armpit. BIA-ALCL may occur several years after breast augmentation. Other symptoms associated with BIA-ALCL include:
- Enlargement of the breast implant surgery
- Breast hardening
- Pain in the armpit or breast
- Skin rash or redness around the breast (a rare symptom)
Diagnosis of BIA-ALCL
To diagnose BIA-ALCL, the doctor will first recommend an ultrasound. This is after the patient develops swelling around the breast or armpits. The ultrasound determines if a collection of fluid is the cause of the swelling. If there’s fluid in the swelling, it is taken for further laboratory analysis to diagnose BIA-ALCL. It’s important to note that BIA-ALCL is rare, and most fluid collection isn’t cancer. If the laboratory test detects the presence of BA-ALCL, the doctor may recommend further tests such as CT scans and MRIs.
Despite the minimal risk of contracting ALCL, the cancer can be fatal and can spread to the rest of the body. However, BIA-ALCL is treatable in the early stages. BIA-ALCL treatment involves the removal of the implant and the surrounding capsule. The surgeon removes both implants even if BIA-ALCL is found on only one breast. Sometimes, if the cancer is severe, the doctor recommends radiation therapy, immunotherapy, stem cell transplant, and chemotherapy treatment.
After implant removal, the patient may undergo reconstruction surgery to replace the implant. Women who have undergone breast augmentation should ensure regular monitoring and watch the symptoms of BIA-ALCL.
Association of Textured Implants and BIA-ALCL
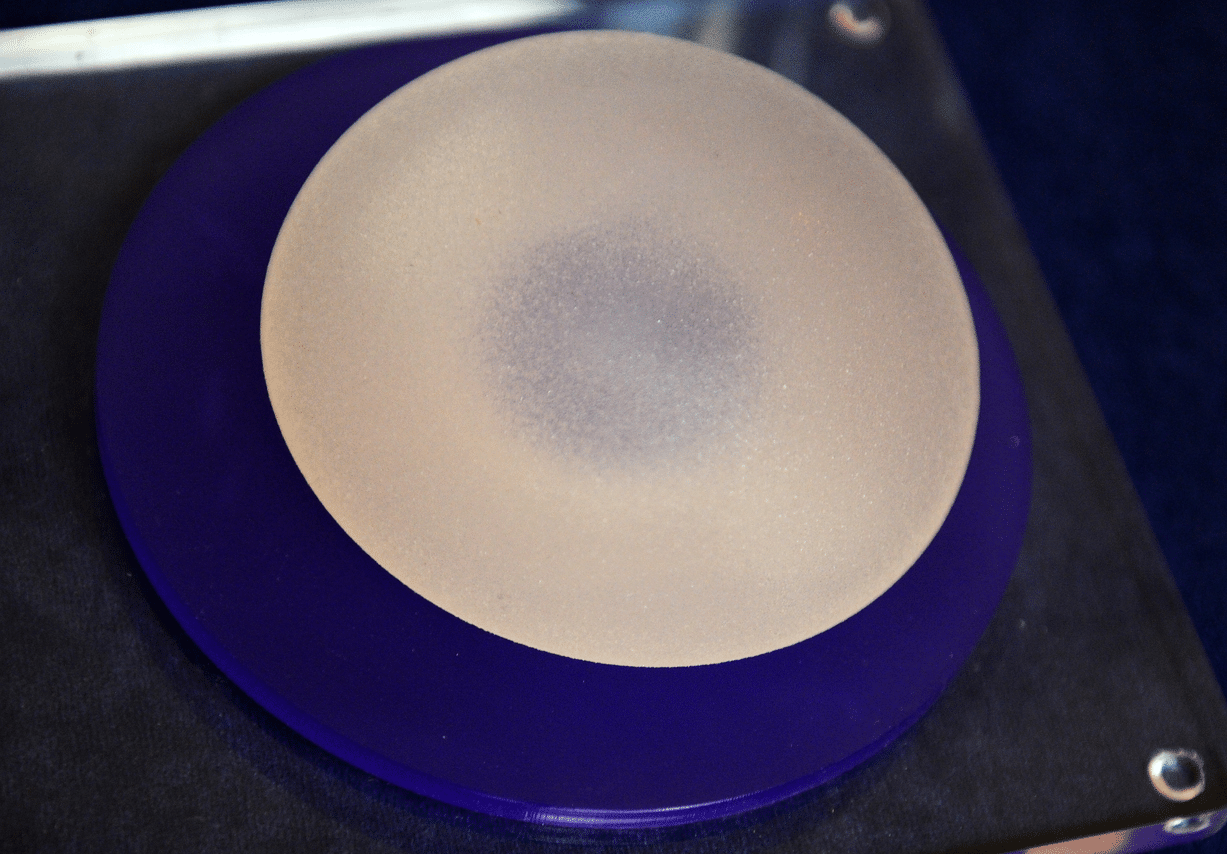
Textured breast implant
Textured breast implants, can be micro-textured or macro-textured. A particular type of macro-textured breast implant is associated with an increased risk of BIA-ALCL. This led to TGA banning the use of Macro-textured implants in Australia.
The theory behind the increased rate of BIA-ALCL in textured implants suggests that the rough surface of the implant may cause chronic inflammation, leading to cancer. Another theory suggests that the rough implant’s surface creates an area for bacterial growth, creating a biofilm. The biofilm causes inflammation, leading to lymphoma. In addition to chronic inflammation and bacterial contamination, researchers link BIA-ALCL cancer to genetic mutations. Therefore, some individuals are more prone to BIA-ALCL than others.
There are no proven ways of preventing BIA-ALCL. Therefore, the patient should ensure early detection of the complication before it becomes fatal. Patients with the banned implants don’t have to remove them. However, they should be aware of BIA-ALCL symptoms and regularly monitor the area around the breast implant.
If patients notice any change around the breast, they should seek medical check-ups as soon as possible. It’s important to note that while mammograms are crucial in breast cancer detection, they don’t detect BIA-ALCL.
Implant Rupture

Ruptured breast implant
Breast implants are prone to rupture or deflation. Rupture occurs in all breast implants, while deflation only occurs in saline-filled breast implants.
Silicone breast implants are associated with silent ruptures, which are hard to detect. Silent ruptures don’t affect the breast’s look and feel. Doctors use MRIs to detect silent ruptures in silicone gel implants. When the implant ruptures, the silicone gel spills through the rupture but stays within the capsule. This is known as intra-capsular rupture. However, there are times when the silicone gel moves to other body parts, a condition known as extra-capsular rupture. Extra-capsular rupture makes it hard for the plastic surgeon to remove the silicone gel implant.
Despite silicone implants having silent ruptures, there are occasions when the breast may decrease in size and shape. Also, there may be noticeable lumps around the implant, breast tenderness and pain, breast unevenness, swelling, tingling, numbness, or a burning sensation.
When saline implants rupture, the saline solution inside the implant leaks, deflating the implant. This will lead to loss of breast size and shape. Some surgical procedures are not recommended for saline breast implants to prevent and reduce the risk of rupture. These include:
- Closed capsulotomy
- Contact of the saline implant with Betadine
- Injections onto the implant shell
- Inserting more than one implant into the breast pocket
- Placement of substances other than saline solution inside the implant
- Altering the implant shape and size
Treatment of ruptured implants involves the removal of the ruptured implant. Below are some of the common causes of implant rupture:
- Capsular contracture
- Implant aging
- Damage by surgical tools during insertion
- Physical trauma on the implant
- Underfilling/overfilling saline breast implants
- Compression of the implant during mammograms
- Damage during fluid drain and biopsies
- Excessive handling during insertion
- Use of unapproved insertion procedures
Additional Surgery

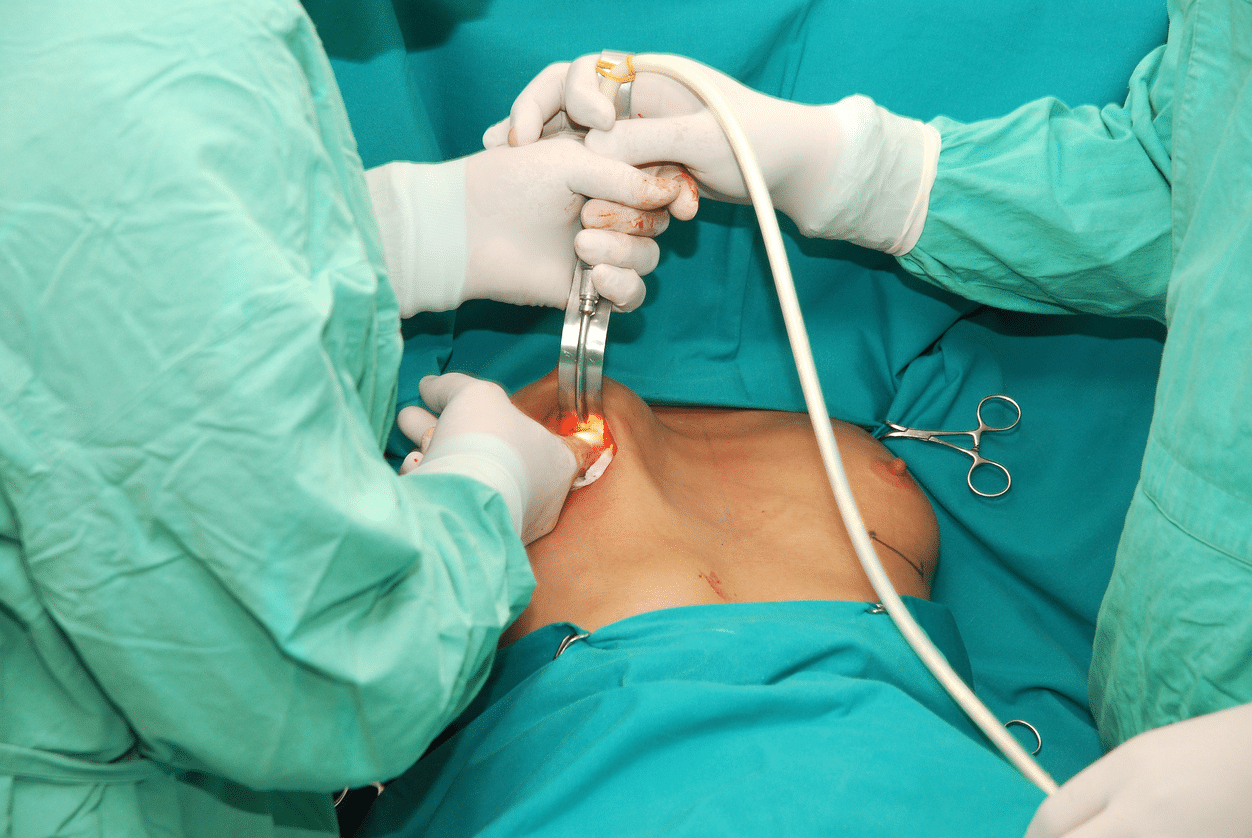
Breast Augmentation Surgery
The patient may have to undergo additional surgeries due to implant complications. Also, the procedure’s outcomes may be unsatisfactory to the patient, and they may request revision surgery. The additional surgery type depends on the reason for re-operation and the desired results. Types of other surgeries performed on patients may include:
- Removal of the capsule and scar tissue surrounding the implant
- Implant removal due to rupture or treatment of complications like BIA-ALCL
- Scar revision to remove excess noticeable scar tissue
- Implant repositioning due to implant malposition and asymmetry
- Biopsy for cyst removal
- Draining of excess fluid in the capsule
Implant Rotation & Malposition

Teardrop breast implant
Implant malposition is a condition where the implant moves from its original position. The implant may also rotate, and the back faces to the front. Implant rotation distorts the breast shape. Breast malposition and rotation often occur when the implant is smaller than the breast pocket or vice versa.
The complication is common with smooth implants because they can move freely in the breast pocket. Textured implants provide a surface for integration between the implant and the breast tissue, reducing implant movement. This, in turn, reduces implant malposition.
The different types of breast malposition include the implants sitting too low, too high, on the armpit, or close together. In addition, Malposition may cause the breast to move too close, causing symmastia. This condition is where the breasts are very close and thus look like one. On rare occasions, the skin at the centre of the breasts may rise above the breastbone.
Implant malposition will cause asymmetry in the breast and nipples and a change in breast shape, whether standing or lying. The breast may also feel different when touched. Treatment of breast malposition involves revision surgery to reposition the implants and tighten the breast pockets.
Implant Related Illnesses
Breast implant illnesses are illnesses related to breast implants. Despite patients experiencing numerous symptoms after breast augmentation, no research directly links the symptoms and breast implants. Some signs of breast implant illnesses include:
- Depression or anxiety
- Chronic fatigue
- Brain fog
- Hair loss
- Muscle and joint pain
- Weight changes
- Headaches
- Skin rashes
- Hormonal issues
Research is ongoing regarding these symptoms to determine their relationship with breast implants. Therefore, patients experiencing these implant-related illnesses should report them immediately and include the manufacturer’s name, implant brand name, and details of the symptoms.
Other Breast Implant Complications
Breast implants are associated with numerous major and minor complications apart from the ones discussed above. So, what else do we have?
- Breast Asymmetry: This is the unevenness in the shape and size of the breasts. Several factors, including implant malposition, rupture, and capsular contracture, may cause breast asymmetry.
- Seroma: The condition occurs when fluid collects around the breast implant. It may cause pain, bruising, and swelling. Large amounts of fluid collection require a surgical drain to remove.
- Rippling and wrinkling of the breast
- Skin rashes around the implant area
- Temporary numbness around the breast
- Patients may experience increased/decreased nipple sensation due to nerve damage. This may include nipple pain.
- Breast skin shrinking and thinning
- Lack of proper wound healing
- Visibility of the implant, especially in patients with insufficient breast tissue
- Infections like toxic shock syndrome
- Prospective pain after the surgery. The pain is mainly mild and is regulated by medication. However, the pain may become severe, requiring medical attention.
- Damage of the breast tissue during surgery and insertion
- Noticeable scarring
- Excessive bleeding during the surgery
- Tightness around the chest
- Breast sagging due to weight loss, age, or pregnancy
- Lumps around the implant due to calcium deposits
- Allergic anesthesia reactions.
There’s no association between breast implants and breast cancer (except BIA-ALCL see above), reproductive problems, or connective tissue disease. Breastfeeding may be difficult after breast augmentation since milk-producing glands may be affected during the surgery. However, some women usually breastfeed even after undergoing breast augmentation.
Does Breast Implant Complications Lead to Implant Removal?
Breast implant removal is a crucial decision for women with breast implants. Breast implant complications can lead to implant removal, with or without replacement. Some women will remove their implants without reason, of their own free will, while others for medical reasons.
There are different methods of implant removal. The first method involves the removal of the implant, leaving the scar capsule that surrounds the implant. The procedure has less surgical dissection. Another method called en-bloc capsulectomy, involves removing the implant and the whole scar capsule without cutting the capsule.
The other method involves cutting the scar capsule and removing the implant, followed by most or all of the scar capsule.
Removing the breast implant without replacement leads to breast sagging, dimpling, puckering, and chest-wall concavity. Significant deformities can occur in women with large implants whose implants are removed.
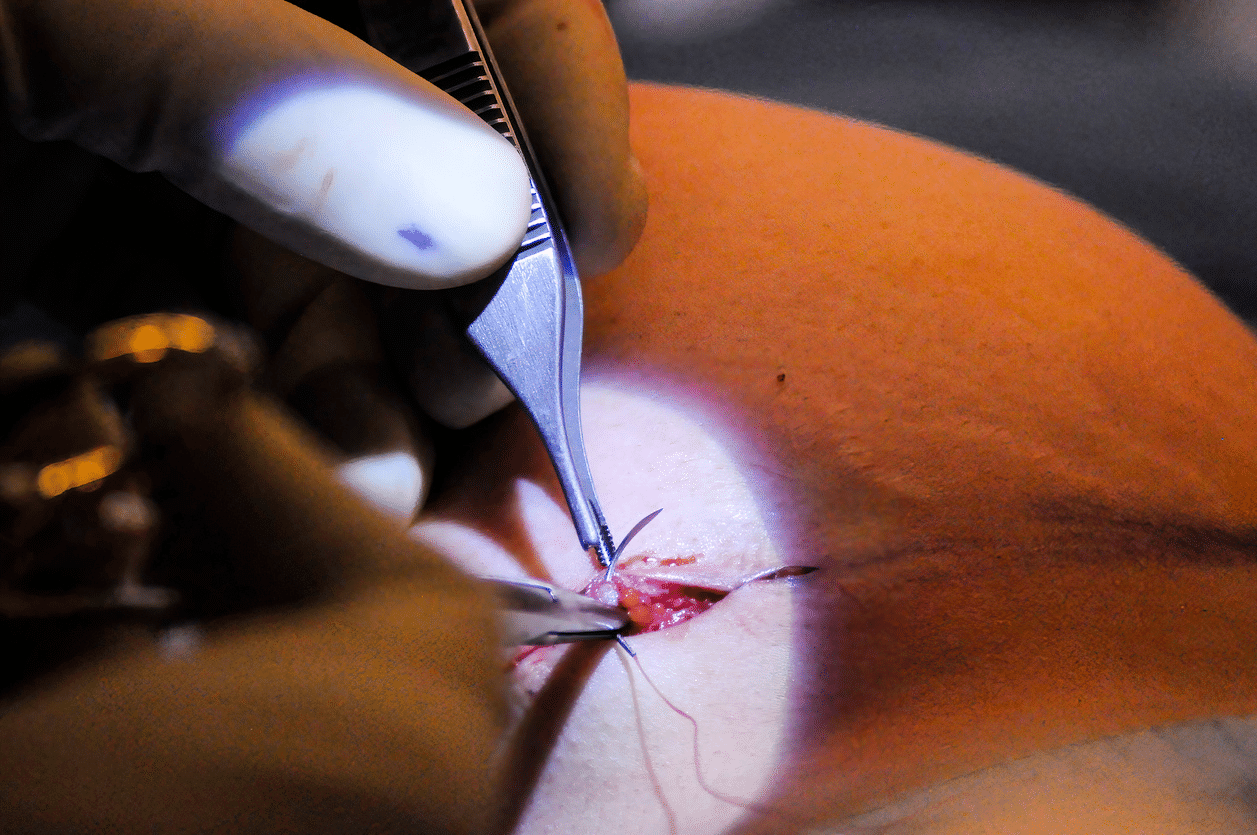
Common Symptoms Women Experience After Breast Surgery
To place the implant into the breast tissue, the surgeon makes an axillary (under the arm), periareolar (around the nipple), or inframammary (under the breast) incision. The surgeon then creates a breast pocket and inserts the implant. After surgery, the patient will experience swelling and soreness for a few days or weeks.
The healing will take place, leaving a scar that reduces with time. The surgeon may advise the patient to wear a sports bra or compression bandage to support the breasts. Note that the breast may be sensitive to touch and painful during healing. In addition, the patient may notice skin redness around the implant.
Things to Consider Before Undergoing Breast Augmentation
In addition to learning the risks involved in breast augmentation, patients should consider the following before getting breast implants.
- Breast implants do not have a lifetime guarantee. Factors like weight loss and gain may also affect how the breast looks. In addition, aged implants have a higher risk of rupture.
- Breast implants don’t prevent breast sagging. Therefore, the surgeon may recommend mastopexy, a breast lift procedure, in addition to breast augmentation.
- Removal of breast implants without replacement will likely cause the breasts to appear saggy.
- The implants may interfere with the breast tissue causing breastfeeding challenges.
- Perfect results are not guaranteed, and the patient may be dissatisfied after the procedure.
- Revision procedures are more complicated than primary procedures and may result in nerve damage and poor healing.
- There may be additional charges relating to breast augmentation complications. These include extra surgeon, hospital, and anesthesia fees.
- The patient may be subjected to additional procedures from those discussed with the surgeon in case of unforeseen conditions during the procedure.
- The insurance may not cover breast augmentation and most additional procedures unless medically necessary. This means the patient should be prepared to pay additional costs.
Regulations Put in Place to Ensure Patient Protection
Different health regulatory bodies in Australia, including TGA and AHPRA, have established regulations to regulate breast augmentation in Sydney. The regulations aim to increase patient safety and protect them from lack of information, malpractices, and unauthorised implants.
Regulations require manufacturers to include breast implants in a boxed package, listing the potential risks of breast implants on the packaging. Manufacturers should also sell breast implants to medical practitioners who analyse the side effects and potential risks.
On the side of health practitioners, they should thoroughly discuss the risks associated with implants with their patients. In addition, women with breast implants should undergo regular screening. Routine screening can identify complications early for treatment.
References
- DePaola, N. E. K. (2019, February 1). Breast Implant–Associated Anaplastic Large Cell Lymphoma: What We Know. PubMed Central (PMC).
- Gabriel, S. E., Woods, J., O’Fallon, W. M., Beard, C. J., Kurland, L. T., & Melton, L. J. (1997). Complications Leading to Surgery after Breast Implantation. The New England Journal of Medicine, 336(10), 677–682.
- Kim, Y., Kim, Y. S., & Cheon, Y. K. (2014). Prevention of Implant Malposition in Inframammary Augmentation Mammaplasty. Archives of Plastic Surgery, 41(04), 407–413.
- Steinbach, B. G., Hardt, N. S., Abbitt, P. L., Lanier, L. L., & Caffee, H. H. (1993). Breast implants, common complications, and concurrent breast disease. Radiographics, 13(1), 95–118.
- Nahabedian, M. Y. (2019). Round Form-Stable Breast Implants. Plastic and Reconstructive Surgery, 144, 73S-81S.
- Flores, T., Kerschbaumer, C., Jaklin, F. J., Rohrbacher, A., Weber, M., Luft, M., Aspöck, C., Ströbele, B., Kitzwögerer, M., Lumenta, D. B., Bergmeister, K. D., & Schrögendorfer, K. F. (2023). Gram-positive bacteria increase breast implant related complications: Prospective analysis of 100 revised implants. Plastic and Reconstructive Surgery, Publish Ahead of Print.
- Silicone gel breast implant failure and frequency of additional surgeries: analysis of 35 studies reporting examination of more than 8,000 explants. (1999). PubMed.
- Headon, H., Kasem, A., & Mokbel, K. (2015b). Capsular Contracture after Breast Augmentation: An Update for Clinical Practice. Archives of Plastic Surgery, 42(05), 532–543.