Breast Implant Rupture
Breast augmentation involves using breast implants or fat transfer techniques to enhance breast size and projection. Implant-based breast augmentation is the most common procedure but comes with potential post-surgical complications, such as breast implant rupture. Regardless of whether a patient has saline or silicone implants, all breast implants have an outer silicone shell that can tear or break, causing the silicone or saline solution inside to spill out. The type of implant used in breast augmentation is a factor to consider when it comes to implant rupture. Saline implants tend to leak faster than silicone implants in the event of a rupture. However, modern implants have significantly reduced the incidence of breast implant rupture.
Silicone Breast Implants Rupture
Silicone breast implant rupture occurs when the silicone implant shell breaks, causing the silicone gel inside the implant to leak. The gel leaks gradually to the surrounding breast tissue and may spread to the lymph nodes. Silicone implant ruptures are asymptomatic and hard to detect. Occasionally, patients may experience tenderness and pain on the affected breast and changes in contour.
The categorisation of silicone breast implant rupture depends on the level of silicone leakage. After breast augmentation, the body forms scar tissue, called a capsule, around the implant. This is the body’s defence mechanism against foreign material. The capsule can contain silicone leakage, or the silicone might leak outside the capsule. Below are the two types of silicone implant ruptures.
Intracapsular Rupture
It occurs when the implant’s outer shell ruptures or tears, and the silicone gel leaks into the capsule. The silicone is contained within the capsule and doesn’t leak to the surrounding tissues. This type of rupture is completely asymptomatic and is known as a silent rupture.
Extracapsular Rupture
Occurs when the silicone gel gets past the fibrous capsule into the surrounding tissues. Extracapsular rupture is uncommon and riskier than intracapsular rupture. When the silicone gel leaks into the surrounding tissues, it causes tissue reactions and scar formation, causing noticeable symptoms, including palpable lumps on the breast and pain or changes in breast sensation.
Extracapsular rupture is an advancement of intracapsular rupture, which means that for the silicone gel to leak through the capsule (extracapsular), it’s also in the capsule (intracapsular). Extracapsular rupture is detectable through mammograms or physical examination. However, it is difficult to remove silicone gel from the body tissues.
Newer-generation silicone implants with cohesive gel have a reduced risk of extracapsular contracture. It is important to note that the cohesive silicone gel does not leak into the surrounding tissue.
Common Signs and Symptoms of Ruptured Silicone Breast Implants

So, how do you know you have a ruptured silicone breast implant? Here are some signs and symptoms to watch out for.
Breast Tenderness or Pain
Pain may result from silicone pushing through the fibrous capsule into the surrounding tissue. It can also result from inflammation, causing breast tenderness.
Breast Lumps
The silicone may interact with the body tissues resulting in granulomatous tissue formation and inflammation. This leads to the formation of lumps around the breast. However, lumps resulting from silicone implant rupture take a while to develop. Lumps on the breast may not necessarily signify implant rupture. Therefore, on discovering a lump on the breast, a patient should undergo a clinical examination to determine the cause.
Deformed Breast
A ruptured silicone implant is hard to notice because it doesn’t cause any change in breast implant shape since the body doesn’t absorb the silicone gel. The silicone stays in place despite the rupture. Therefore, the body creates a barrier of scar tissue known as siliconoma or granulomas to prevent the silicone gel from slipping into other body parts. As the silicone gel keeps getting out of the implant, the protective scar tissue grows hard, squeezing the implant. This affects the breast shape and leads to significant breast deformity.
Lymphoma
Lymphoma is cancer affecting the lymphatic system. Some silicone breast implants have been reported to result in lymphoma in rare cases. Therefore, the surgeon should query the patient on systemic symptoms and local or axillary masses that could signal lymphoma.
Abnormally Soft or Firm Breasts
This is because as the silicone gel leaves the implant, the breast becomes softer. However, as a tissue capsule forms, the breast may become firmer.
Increased Silicone Levels
Increased silicone levels in the body may result in additional symptoms like fever, anaemia, rashes, and kidney issues.
Saline Breast Implants Rupture
Saline breast implant rupture is also known as deflation. When a saline implant’s outer shell ruptures, the solution leaks out of the implant gradually, causing significant deflation within a few days. The patient can immediately notice ruptured saline breast implants due to the decreased breast size and rippling.
Unlike the silicone gel, the saline solution is sterile, harmless and absorbed into the body. However, in cases of any bacterial infection in the implant, it can lead to health problems. The rupture may result from a failed valve if the implant ruptures after a few weeks following breast augmentation.
Common Signs and Symptoms of Ruptured Saline Breast Implants
Here are some common signs of ruptured saline breast implants.
Changes in Breast Volume, Size, and Shape
Saline implant rupture causes breast implant deflation within 2 to 3 days. This reduces breast size and volume, causing notable differences between the unaffected and affected breast. The volume change will affect the breast shape.
Breast Tenderness or Pain
All types of breast implant ruptures are likely to cause breast tenderness. However, most patients with ruptured saline breast implants rarely experience breast pain. However, there are instances where the patient may experience pain resulting from the rapid change in breast volume or post-traumatic ruptures.
Rippling
Deflation of ruptured saline implants causes visible ripples on the breast. This sometimes results from the ruptured implant folding over itself.
When the surgeon conducts surgery to remove the ruptured implant early after deflation, they will find some saline solution inside the capsule. However, if the surgery takes long, the body will absorb the saline solution leaving only the remains of the ruptured implant.
What are the Causes of Implant Rupture?

Below are the causes of breast implant rupture.
- Normal aging. Breast implants are not lifetime devices; most require a change after 10 to 20 years. As the breast implants age, wear and tear may lead to implant rupture.
- Physical trauma. Intense physical stress or trauma to the breast can result in breast implant rupture. Regular physical activities are unlikely to cause implant rupture.
- Capsular contracture. The thick scar tissue from capsular contracture can tighten and squeeze the implant, causing a rupture. Severe capsular contracture can lead to secondary implant rupture.
- Compression during a mammogram. Compressions applied during mammogram breast screening can lead to ruptured implants. However, this is unlikely in newer-generation implants.
- Damage by surgical instruments. The surgeon may accidentally perforate the implant with surgical tools during insertion. This affects the implant integrity as these microscopic perforations may enlarge with time, causing implant rupture. Damage by surgical instruments is the most frequent cause of implant rupture, with 51-64% compared to 35-37% in ruptures with no evidence of damage by surgical instruments.
- Shell swell. This is a condition where the implant’s shell decreases strength over time due to silicone migration into the shell. There is conflicting data on whether implants undergo shell swell and whether it leads to implant rupture.
- Injury during certain surgical procedures. The implants may get a perforation during breast procedures like fluid drainage and biopsies, leading to a rupture.
- Closed capsulotomy. This technique helps treat capsular contracture by squeezing the breasts manually from the outside to break the fibrous capsule. However, too much pressure may cause a rupture of saline breast implants.
- Injection through the saline implant shell
- Manufacturing defects
- Incompetent valves in saline breast implants
- Implant folding
Overfilling or underfilling saline breast implants is unlikely to cause implant rupture, although adhering to the filling guidelines is essential. In addition, non-intense breast implant manipulation and physical contact doesn’t cause implant rupture. This also applies to sneezing or coughing.
Diagnosis of Breast Implant Rupture

If a patient notices breast rupture symptoms, the first step is to contact a specialist surgeon and undergo a physical exam. Saline implant rupture can be diagnosed through this means without radiography because it leads to noticeable changes in breast size. Some considerations during implant rupture examination include the date of implant placement, the type of breast implant used, and the duration of symptoms.

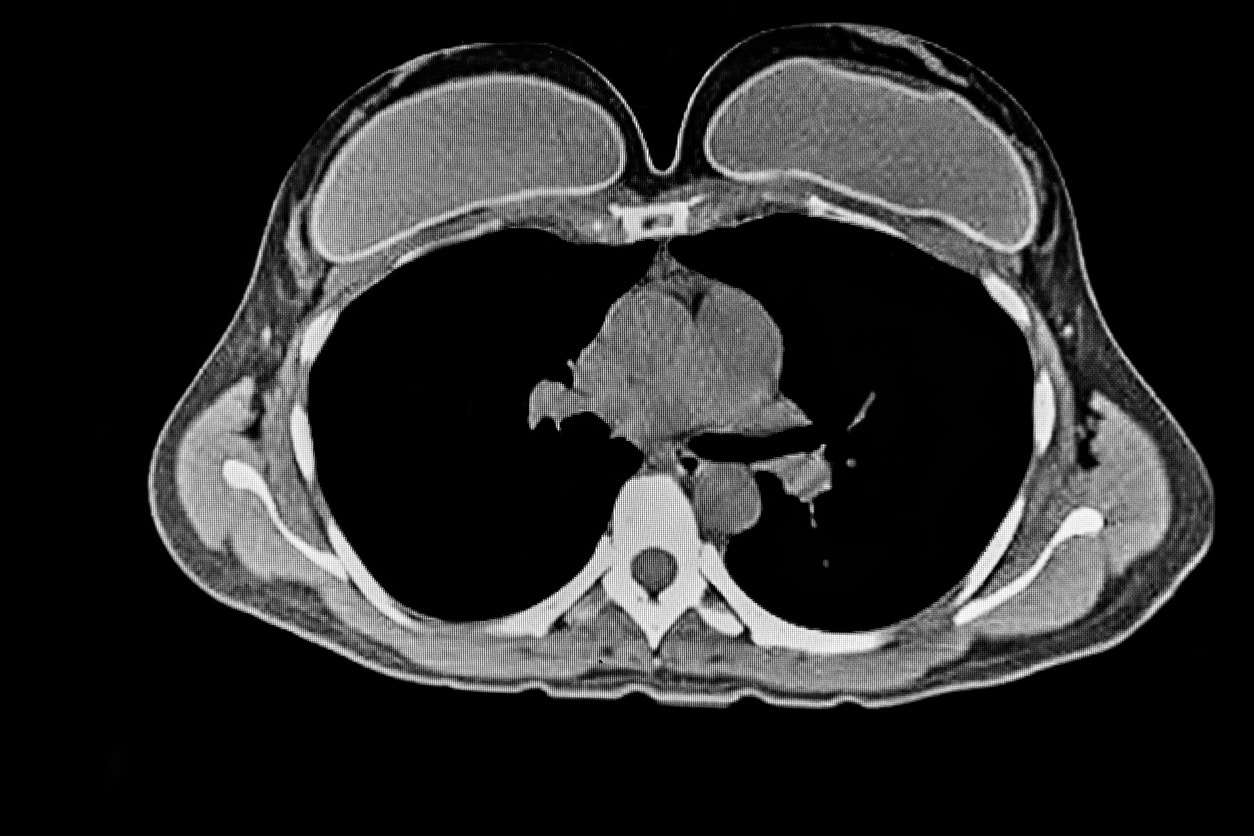
Sometimes, the surgeon may recommend an MRI (Magnetic Resonance Imaging), Ultrasound, or mammography to detect implant rupture.
When mammography detects ruptured saline implants, the implant appears wrinkled. When using ultrasound, an intact implant will show a simple anechoic interior, while a ruptured implant will show wrinkles or folds.
Intracapsular ruptures are hard to detect through physical examination, mammography, or ultrasound. MRI is the most effective method of detecting intracapsular rupture, but it’s expensive compared to the other methods. On the other hand, extracapsular ruptures are detectable using ultrasound and mammography.
However, MRI determines the extent of the silicone leakage (extravasation). Ultrasound doesn’t have the sensitivity to detect intracapsular silicone ruptures because the silicone is hypoechoic. In addition, non-contrast MRI can differentiate between saline and silicone implants using water or silicone-only sequences.
Since silicone implant ruptures are hard to notice, patients with silicone implants should undergo regular breast screening after 2 years after the plastic surgery.
What are the Treatment Options for Ruptured Breast Implants?

The standard treatment for ruptured breast implants includes revision surgery or explanation. Revision surgery involves removing the ruptured implant and implant-based breast reconstruction, while explantation involves implant removal without replacement.
Ruptured silicone implants, whether intracapsular or extracapsular, should also be removed immediately upon detection. This is to prevent silicone migration to the lymph nodes. Replacement should involve newer generation implants with cohesive silicone that doesn’t migrate in case of implant rupture. In ruptured saline implants, the surgeon should remove the empty shell.
The surgeon can perform a capsulectomy to remove the implant and the fibrous capsule. Extracapsular rupture is hard to treat, and the surgeon may recommend several surgeries to remove all the silicone. If a patient considers explantation, the surgeon may suggest a breast lift procedure (mastopexy) to reduce breast sagging and restore breast projection.
Apart from the two treatments, a patient may consider reconstruction using a fat transfer technique. The process involves getting fat from other body parts like the belly and thighs using liposuction and injecting it into the breast. The procedure offers a more natural alternative to breast reconstruction with implants. Fat transfer eliminates the risk of future breast implant complications.
Health Impacts of Ruptured Breast Implants

Most patients are concerned about the health risks of a ruptured breast implant. The saline solution is sterile and doesn’t cause any harm to the body unless there is an initial bacterial infection in the implant.
There are concerns about the health risk posed by possible silicone migration to the lymph nodes. However, research shows that implant rupture is not associated with autoimmune disease. In addition, ruptured silicone implants aren’t known to cause reproductive problems, breast cancer, or connective tissue disease.
What is the Likelihood of Implant Rupture?
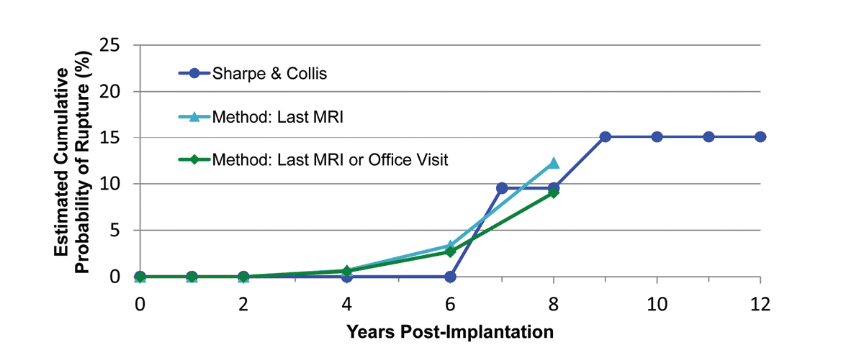
Source: Handel N et Al. “Breast implant rupture: causes, incidence, clinical impact, and management.”, Plastic & Reconstructive Surgery. 132(5):1128-1137, 2013 Nov.
A breast implant can rupture at any time after breast surgery. The longer the implant’s duration inside the body, the higher the likelihood of rupture. However, it’s impossible to determine the likelihood of implant rupture accurately. This is because of the wide range of breast implants from different manufacturers and the rapid advancement of implant generations. Also, there’s no long-term data on the rate of implant rupture. Modern breast implants are less likely to rupture than older-generation implants.
How Long Can You Stay with a Ruptured Breast Implant?
It’s not safe to leave ruptured silicone implants in place after detection. The surgeon should remove the implants and the scar capsule if it’s also affected. If you have only one ruptured implant, the surgeon can recommend the removal of both implants.
In cases of a ruptured saline implant, the surgeon can remove it immediately or recommend waiting until you are ready for surgery to remove the implant. You can choose between explantation and breast removal, with replacement as a treatment option for ruptured implants.
Final Take
Breast implant rupture is a breast implant complication associated with both therapeutic and cosmetic augmentation. Breast implant rupture can occur any time after undergoing breast surgery, and there’s no accurate method to determine the probability of occurrence of implant rupture. This is due to differences in breast surgery methodologies, lack of enough data, and availability of many implants from different manufacturers.
Treating ruptured implants involves implant removal upon detection and replacement with modern implants or implant removal without replacement. This depends on the patient’s choice or the underlying risks.
References
- Fosheim, K., Bojesen, S., Troestrup, H., & Lænkholm, A. V. (2022b). Capsulectomy Can Successfully Treat Chronic Encapsulated Breast Seroma: A Case Report. Cureus.
- Hillard, C. J., Fowler, J. D., Barta, R. J., & Cunningham, B. A. (2017). Silicone breast implant rupture: a review. Gland Surgery, 6(2), 163–168.
- Safran, T., Nepon, H., Chu, C. K., Winocour, S., Murphy, A. C., Davison, P., Dionisopolos, T., & Vorstenbosch, J. (2021). Current Concepts in Capsular Contracture: Pathophysiology, Prevention, and Management. Seminars in Plastic Surgery, 35(03), 189–197.
- Swezey, E. (2023, January 16). . StatPearls – NCBI Bookshelf.
- Ezmas, M. N., Norlia, A., Suraya, A., Adnan, W. a. W., & Looi, L. (2022). Silicone From Pectoralis Muscle Contraction Causing IgA Nephropathy: A Case Report. Frontiers in Oncology, 12.
- Nam, S. E., Bang, B. S., Lee, E. K., Sung, J., Song, K. B., Yoo, Y. B., Park, D. W., & Kim, J. H. (2023). Use of High-resolution Ultrasound in Characterizing a Breast Implant and Detecting a Rupture of the Device Before Reoperation in Women Receiving Augmentation Mammaplasty. Plastic and Reconstructive Surgery, 152(1), 39–43.
- Hölmich, L. R., Lipworth, L., McLaughlin, J. K., & Friis, S. (2007). and Connective Tissue Disease: A Review of the literature. Plastic and Reconstructive Surgery, 120(Supplement 1), 62S-69S.
- Lipworth, L., Tarone, R. E., & McLaughlin, J. K. (2004). Silicone breast implants and connective tissue disease. Annals of Plastic Surgery, 52(6), 598–601.
- Handel, N., Garcia, M., & Wixtrom, R. N. (2013b). Breast implant rupture. Plastic and Reconstructive Surgery, 132(5), 1128–1137.