Can I Breastfeed After Breast Implants
Women who have undergone breast implant surgery can often successfully breastfeed their babies. While there may be potential challenges, such as 25% decreased milk production and nipple sensitivity, many women with breast implants have provided their infants with the vital benefits of breastfeeding.
Despite the worldwide popularity of implants, numerous myths and insufficient information regarding the associated side effects exist. One of these is breastfeeding. This is why one commonly asked question among women is, “Can I breastfeed after a breast implant?’.
This means that women with breastfeeding breast implants or those planning on getting them may have plans to get the babies. Therefore, one of the primary concerns may be whether they can breastfeed after breast implants.
Breast Implants and Breastfeeding
One of the most common theories regarding breast implants is that women cannot breastfeed after breast augmentation. However, most women with breast implants can successfully breastfeed. Even though it’s possible, it’s important to note that breastfeeding with implants depends on various factors, including implant placement, type of incision, and implant size.
In addition, different surgical procedures may affect breastfeeding. Women may find it more challenging to breastfeed after breast reduction and mastopexy (breast lift) because it involves the removal of a part of the glandular tissue.
Other factors include pressure exerted on the lactiferous ducts by implants, and damage to the glandular tissues, nerves, and ducts during surgery. Implant-related complications like capsular contracture, hematoma, and other infections may also affect breastfeeding. Additionally, pain from such illnesses may cause discomfort during breastfeeding.
The doctor cannot guarantee that the patient will breastfeed successfully after breast surgery, and the only way to find out is by the patient breastfeeding the child and monitoring the results. Most women with breast implants can usually breastfeed, but exclusive breastfeeding might be challenging.

Exclusive Breastfeeding
Breast milk provides the essential nutrients in an infant. Exclusive breastfeeding involves giving an infant only breastmilk without mixing it with other liquids, including water, in the first six months. WHO recommends additional breastfeeding to the age of two years in addition to complementary foods. Enough milk is essential for exclusive breastfeeding, which is crucial in supplying the infant with essential body requirements. However, women with low milk supply can use supplements to support breastfeeding.
Breast milk provides the child with all the nutrient requirements in the first six months, more than half of the requirements in the next six months, and one-third of the nutrients in the second year. Colostrum, produced during the first days, is rich in proteins, beneficial compounds and low in sugar. In addition to the nutrients, colostrum helps in the digestive tract development.
Breast milk also contains antibodies that protect the infant from childhood conditions like otitis media, pneumonia, malocclusion, iron deficiency anaemia, diabetes mellitus, and eczema. This improves the child’s health, reducing child mortality and morbidity. In addition, it decreases the number of child deaths. Other advantages of breast milk include:
- Neurodevelopment in infants thus increases the child’s intelligence
- Increasing the mother-child bond
- Promoting healthy weight gain, reducing the obesity rate in babies
- Lowering the risk of SIDS (sudden infant death syndrome)
- Reducing the rate of the ovary and breast cancer, haemorrhage, high blood pressure, and postpartum depression in mothers
- Breastfeeding prevents menstruation in mothers with babies and helps in uterus contraction.
Lack of either mixed or exclusive breastfeeding may affect the child, resulting in neonatal malnutrition, psychomotor development alterations, and psychological and social disturbances. Women with breast implants may find it challenging to establish exclusive breastfeeding due to low milk supply. Studies show a notably reduced rate of exclusive breastfeeding in women with breast implants compared to those without breast implants.
Does the Type of Breast Implant Affect Breastfeeding?
Despite the numerous breast implant advantages, there’s a rising concern about the side effects of implants and whether the type of breast implant affects breastfeeding. The concern is that exposure of the mother to contaminants may cause breast milk contamination. Contamination of breast milk may affect the child’s development and growth. There’s less clinical evidence and studies to prove whether the breast implant type leads to breast milk contamination.
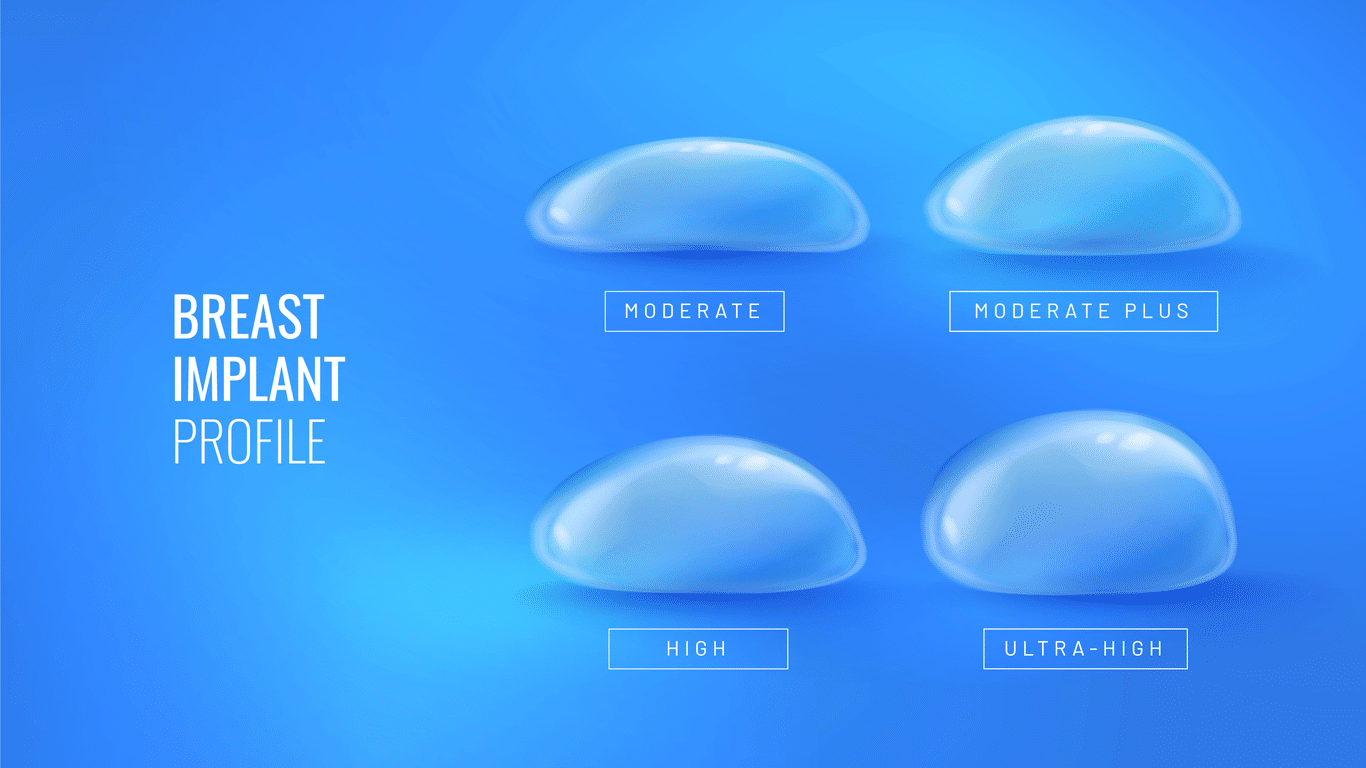
Apart from possible breast milk contamination, breast implants may exert pressure on the breast tissue. Large breast implants on a small chest can result in high pressure on the mammary parenchyma. A lot of pressure on the breast tissue may damage or block the glandular tissue, causing reduced milk production. In addition, the pressure exerted by breast implants may trigger the engorgement feeling (breast full of milk). This signals the breast to produce small amounts of milk.
Silicone gel and saline implants have various side effects and risks, raising breastfeeding concerns. Below are the types of breast implants, their association with breast milk contamination, and their impact on breastfeeding.
Silicone Breast Implants and Their Effects on Breastfeeding

Smooth silicone breast implant
Silicone breast implants are used in breast augmentation surgery for cosmetic and reconstructive surgery. There’s a great concern about breast milk contamination by the silicone gel used in silicone breast implants. This is associated with the possibility of implant rupture, causing silicone leakage (silicone bleed).
Silicone Bleed, also called gel bleed, is the movement of the silicone gel from the implant through the shell into the patient’s body. The movement increases in case of implant rupture. The bleed can be low or high-grade, and the silicone can travel to other body parts.
Transfer of silicone from mother to child through breast milk can cause complications like abnormal esophageal motility. However, there’s not enough evidence to support that there are silicone deposits in breast milk from lactating mothers with silicone implants. Research indicates no notable silicone level differences in breast milk from women with silicone implants compared to those without implants. The study notes more silicone amounts in baby formula and cow’s milk than in breast milk from women with silicone implants.
Saline Breast Implants and Breastfeeding
Saline breast implants contain a saline solution inside the silicone outer shell. The implants are associated with various risks, including implant rupture. However, there’s no evidence showing that saline solution causes contamination of the breast milk.
However, there’s a notably reduced breastfeeding rate in women with saline breast implants compared to women without breast implants. Despite the reduced rate, the difference is related to factors affecting all breast implants, not just silicone breast implants. These include pressure on the breast tissue, implant-related complications, and damage to the breast nerves during breast surgery.
Surgical Factors Affecting Breastfeeding

Surgical complications will likely damage the mammary tissue and cause pain, affecting breastfeeding. Some of the surgical factors that may affect breastfeeding in women with breast implants include:
- Implant Location
- Type of Incision
- Capsular contracture
- Nipple Sensation
- Proximity of the Implant to the Mammary Glands
- Time Since Breast Surgery
Implant Location
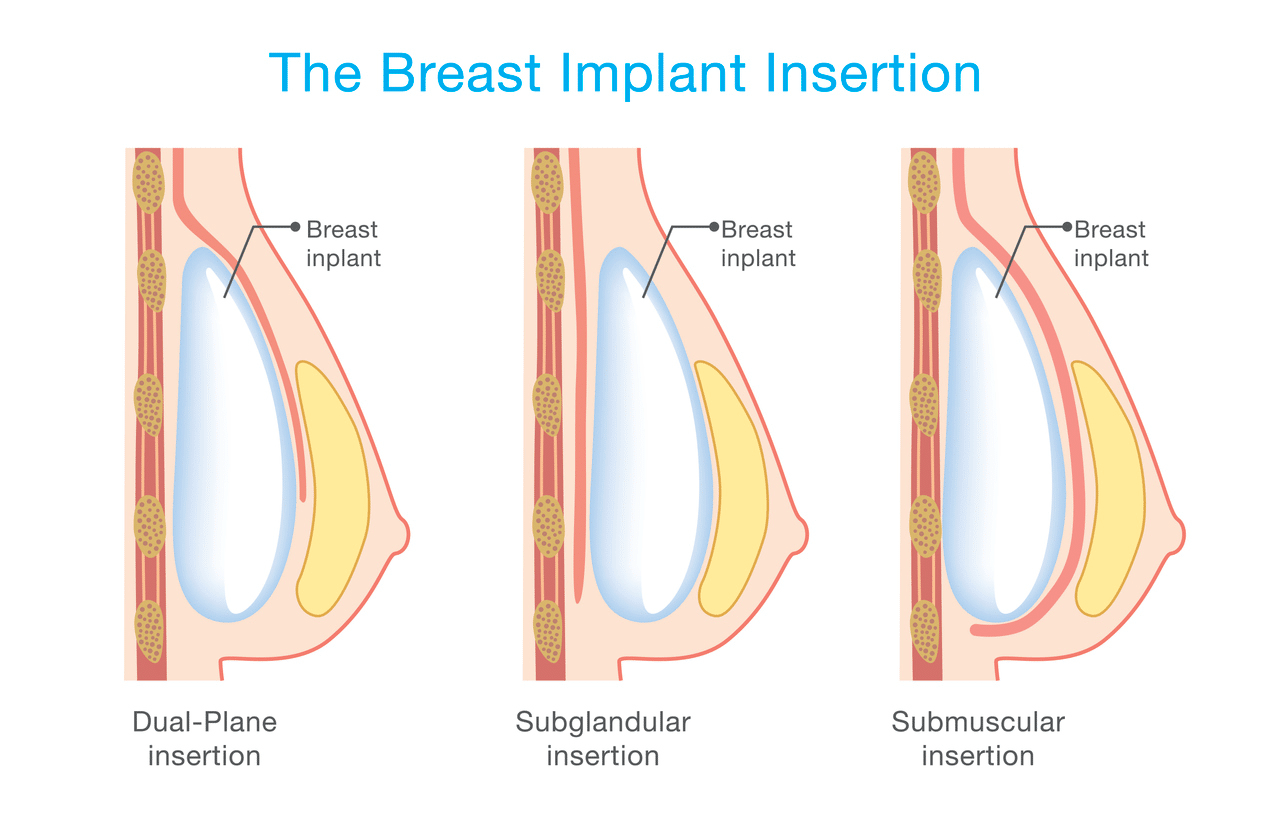
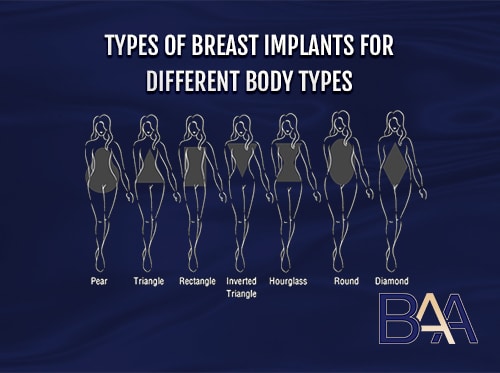
The location of the breast implant plays a crucial role in breastfeeding. The primary types of implant locations include submuscular and subglandular placement. The techniques involve implant placement either between the chest muscle and the glandular tissue or beneath the muscle tissue. Both techniques are associated with different advantages and disadvantages and effects on breastfeeding.
Subglandular technique involves placing the breast implant in front of the chest muscle, behind the breast glands. The technique ensures that the implant doesn’t interfere with the pectoralis muscle and reduces breast movement during arm movement.
However, placing the implant above the mammary glands exerts pressure on the tissue and can block the milk ducts. This makes it challenging for the breast tissues to produce enough breast milk. Women with subglandular placement may find it difficult to achieve exclusive breastfeeding, resulting in the use of supplements.
The submuscular technique involves placing the breast implant beneath the chest muscle. The technique is mainly recommended for lean women because the submuscular placement conceals the implant. It also helps in ensuring firmness of the implants. Breast implants beneath the chest muscle are less likely to interfere with breast milk production. Therefore, women with this technique are expected to achieve exclusive breastfeeding more than those with subglandular placement.
Type of Incision
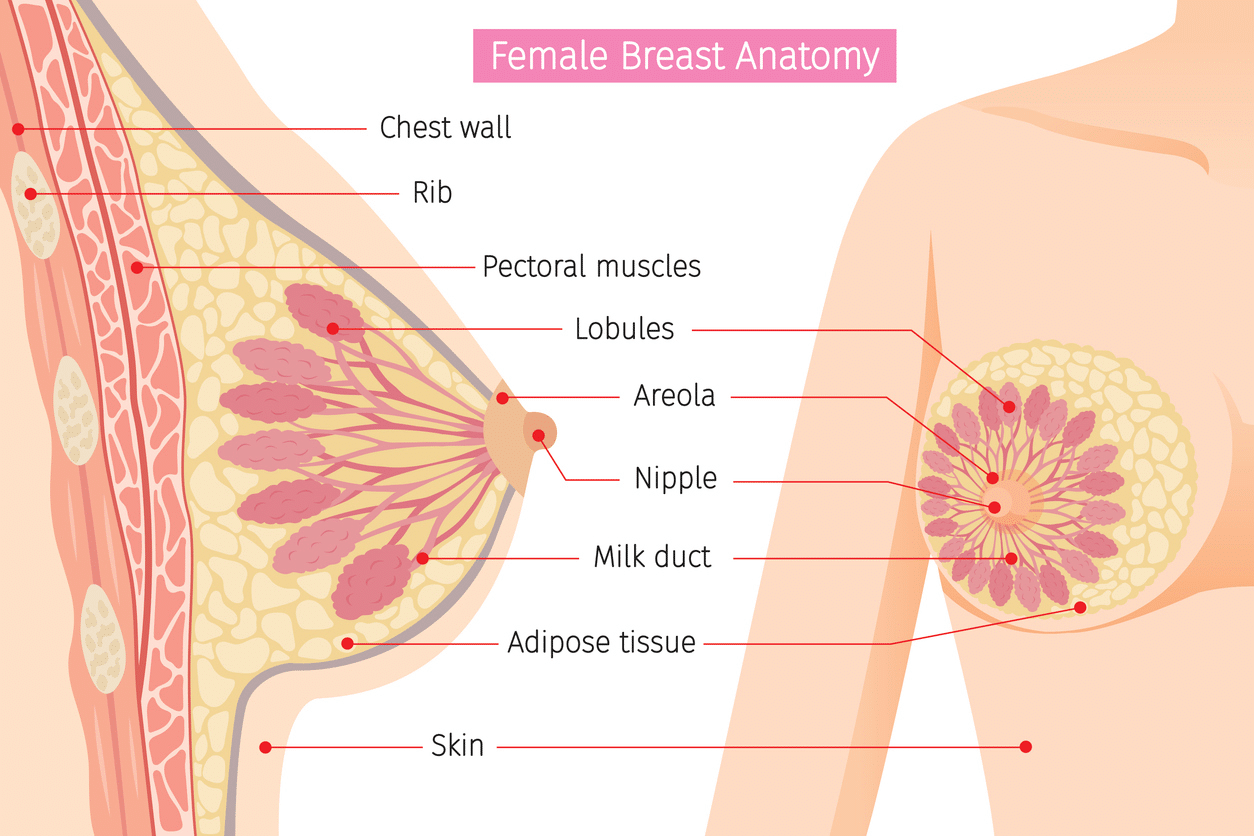
Female breast anatomy
The breast surgeon uses different incisions during breast surgery to create a breast pocket for implant insertion. The main types of incisions used for breast augmentation are periareolar and inframammary. The type of incision used depends on different factors, which the patient must discuss with the doctor during the consultation. There’s a concern that the type of incision used for breast augmentation surgery may damage the breast tissue, affecting breastfeeding.
An inframammary incision is made beneath the breast around the breast crease. The incision allows submuscular, subpectoral, or sub-glandular breast implant placement. Inframammary incisions cause little or no damage to the mammary glands, hence are less likely to affect breastfeeding. This also applies to remote incisions under the armpits or the belly bottom.
A periareolar incision is made around the outer areolar. The incision allows the surgeon to create less visible incisions with reduced scarring. However, periareolar incisions may damage the milk ducts or the nerves. Theories suggest that periareolar incisions damage the galactophorous ducts, however, in rare cases, causing reduced milk drainage and inhibiting milk production. Therefore, there’s a concern that women with periareolar incisions will likely have less milk production, finding it hard to achieve exclusive breastfeeding. However, research shows that periareolar incisions don’t significantly reduce exclusive breastfeeding.
Capsular Contracture
Capsular contracture is a complication resulting from the hardening of the scar tissue around the breast implant. The complication causes stiff breasts and pain, causing inflammation of the breast glands in lactating women. Breastfeeding also increases the risk of capsular contracture in women with breast implants. Pain and inflammation due to capsular contracture may affect milk production and breastfeeding.
Nipple Sensation
Sucking on the nipple directly influences milk production by initiating a reflex to the pituitary gland. The pituitary gland releases oxytocin and prolactin. Prolactin is responsible for milk production, while oxytocin is responsible for milk letdown. However, surgical procedures can cause nerve damage, reducing nipple sensation, which is crucial for milk production.
In addition, surgical procedures may result in pain in the nipple, causing pain during breastfeeding. Nerve damage and the resulting pain can make breastfeeding challenging and uncomfortable for most mothers.
Proximity of the Implant to the Mammary Glands
The distance of the silicone breast implant from the milk ducts can affect breastfeeding. The placement of the breast implant beneath the chest muscle reduces any contact between the implant and the milk-producing ducts.
Theories based on silicone leakage suggest that the closer the implants are to the mammary glands, the higher the chances of silicone getting into the milk ducts. However, there’s no proof of silicone leakage into breast milk in women with silicone breast implants.
Time Since Breast Surgery

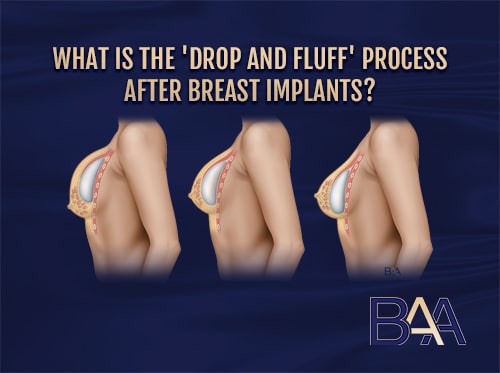
Damaged nerves, glands, and ducts during breast surgery can heal themselves gradually after surgery. The more time passes between getting breast implants and pregnancy, the greater the likelihood that the damaged tissues will heal, producing milk.
However, after several years, the patient may requires revision surgery to replace the breast implants. Revision surgery may further damage the breast tissue, affecting milk production and breastfeeding.
Psychological Factors Affecting Breastfeeding

Women with breast implants may have anxiety about breastfeeding, affecting breastfeeding rates. One of the reasons for anxiety in women with breast implants is the possible contamination of the breast milk. In addition, women with breast implants are concerned about whether breastfeeding may affect breast aesthetics. Therefore, they may be anxious to breastfeed and will likely avoid breastfeeding.
The mother’s intention to breastfeed is another psychological factor affecting breastfeeding in women with breast implants. Women with breast implants are likely to stop breastfeeding when they encounter difficulties. Also, lower self-confidence in breastfeeding and prior expectations may lower the mother’s intention to breastfeed.
Nonsurgical Factors Affecting Breastfeeding
Some nonsurgical factors affecting milk production and breastfeeding include spontaneous pain during nursing, maternal exhaustion, baby-sucking difficulties, stress, nipple injuries, lack of lactation knowledge, or physical stimulations.
To breastfeed successfully, women with breast implants and facing difficulties when breastfeeding should consult a plastic surgeon or a breastfeeding specialist.
Breastfeeding in Women with Hypoplastic Breast Before Breast Augmentation
Insufficient glandular tissue is a primary cause of breastfeeding challenges. In addition, the hypoplastic breast may develop due to the underdevelopment of the breast tissue. The condition is characterised by widely spaced, tubular, or asymmetrical breasts.
Women may undergo breast augmentation to treat hypoplastic breasts. However, an increase in breast size through breast augmentation doesn’t increase the glandular tissue. This means that the glandular tissue will remain underdeveloped and unable to produce enough milk, making breastfeeding difficult.
However, conflicting studies show no relationship between the amount of glandular tissue and milk production. The research indicates that other factors affect the milk quantity produced in lactating mothers apart from breast size. The infant’s demand mainly influences milk production.
How to Successfully Breastfeed with Implants
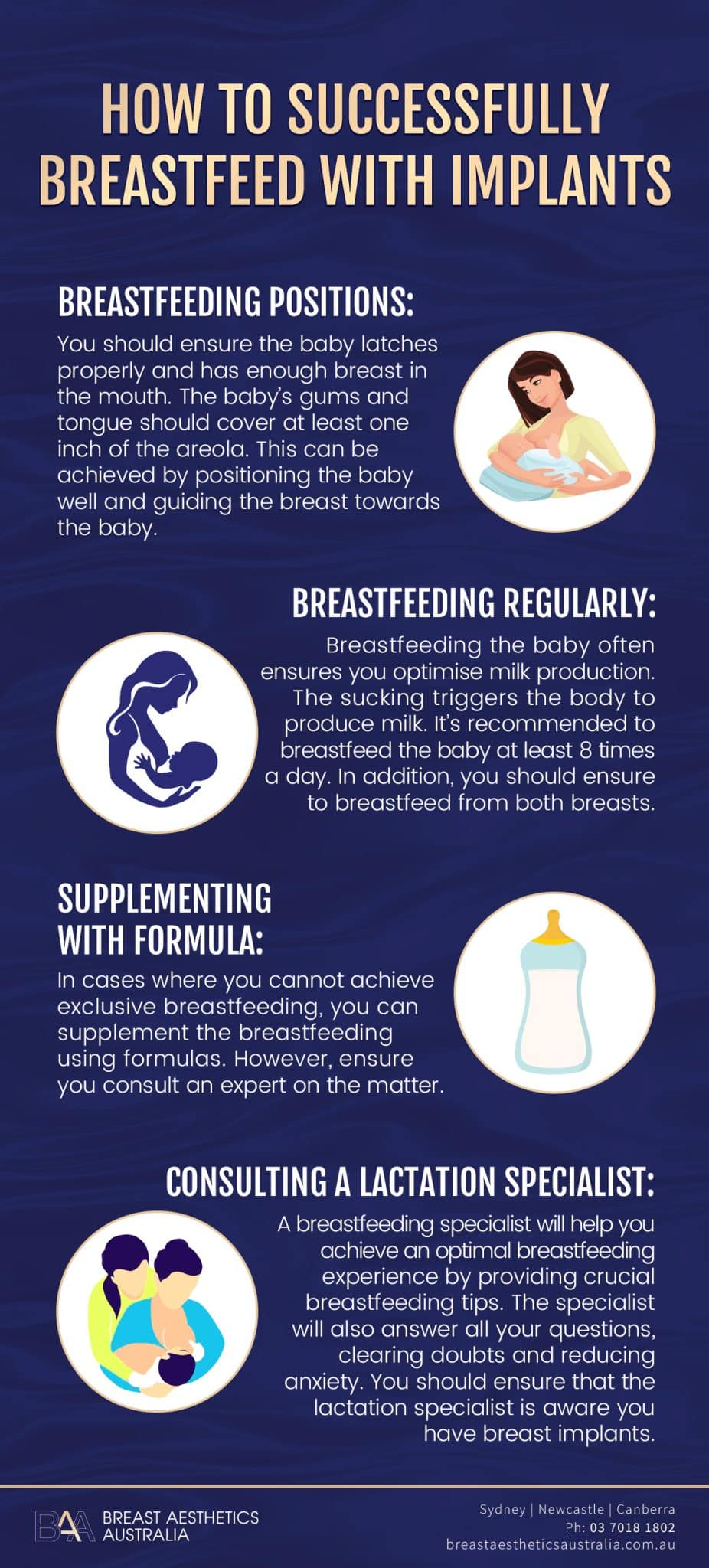
Below are some options to consider for optimising breastfeeding with breast implants.
Breastfeeding Positions: You should ensure the baby latches properly and has enough breast in the mouth. The baby’s gums and tongue should cover at least one inch of the areola. This can be achieved by positioning the baby well and guiding the breast towards the baby.
Breastfeeding Regularly: Breastfeeding the baby often ensures you optimise milk production. The sucking triggers the body to produce milk. It’s recommended to breastfeed the baby at least eight times a day. In addition, you should ensure to breastfeed from both breasts.
Supplementing with Formula: In cases where you cannot achieve exclusive breastfeeding, you can supplement the breastfeeding using formulas. However, ensure you consult an expert on the matter.
Consulting a Lactation Specialist: A breastfeeding specialist will help you achieve an optimal breastfeeding experience by providing crucial breastfeeding tips. The specialist will also answer all your questions, clearing doubts and reducing anxiety. You should ensure that the lactation specialist is aware you have breast implants.
FAQs
There’s a lot of concern about breastfeeding by women with breast implants. Below are some of the frequently asked questions regarding breastfeeding with breast implants.
Will Breastfeeding Ruin the Implants’ Aesthetic Outcome?
Breastfeeding will not affect the implants because the breast tissue protects them. However, the breast shape and size may change due to breastfeeding and weight loss after pregnancy, affecting their aesthetic. The change may be insignificant, and the breast may return to their standard shape after ending breastfeeding.
The amount of change experienced is relative to breast size and weight gained during pregnancy. When the breasts don’t regain shape, some women may undergo further surgery to restore their appearance.
Are There Any Health Concerns Regarding Children Born of Women with Breast Implants?
No clinical reports show any harm to children born by women with breast implants. In addition, there’s no evidence to show any contamination of breast milk in women with silicone breast implants.
Should I First Have Children Before Getting Breast Implants?
You should consult a specialist surgeon when deciding whether to undergo breast augmentation surgery. However, if you’re considering having babies soon, it is probably better to wait before having breast implants to reduce the risks involved. If you have breast implants and are pregnant, or considering getting pregnant, there’s no cause for alarm.
Bottom Line
You can breastfeed after having breast augmentation surgery, and it is safe for the baby to do so. However, studies show up to 25% reduction in breastfeeding rates in women with breast implants vs no breast implants.”
It is essential for individuals considering breast implant surgery to discuss their plans for breastfeeding with their surgeon beforehand, as specific surgical techniques may impact milk production. With proper guidance and support, women can navigate the journey of breastfeeding even after breast augmentation, fostering a strong bond and promoting the health and well-being of both the mother and the baby.
References
- Ajdic, D., Zoghbi, Y., Gerth, D. J., Panthaki, Z. J., & Thaller, S. R. (2016). The Relationship of Bacterial Biofilms and Capsular Contracture in Breast Implants. Aesthetic Surgery Journal, 36(3), 297–309.
- Cheng, F., Dai, S., Wang, C., Zeng, S., Chen, J., & Cen, Y. (2018). Do Breast Implants Influence Breastfeeding? A Meta-Analysis of Comparative Studies. Journal of Human Lactation, 34(3), 424–432.
- Jewell, M. L., Edwards, M. J., Murphy, D. K., & Schumacher, A. M. (2019). Lactation Outcomes in More Than 3500 Women Following Primary Augmentation: 5-Year Data From the Breast Implant Follow-Up Study. Aesthetic Surgery Journal, 39(8), 875–883.
- Filiciani, S., Siemienczuk, G., Nardin, J. C., Cappio, B., Albertengo, A., Nozzi, G., & Caggioli, M. (2016). Cohort Study to Assess the Impact of Breast Implants on Breastfeeding. Plastic and Reconstructive Surgery, 138(6), 1152–1159.
- Chen, C. H. (2017). Cohort Study to Assess the Impact of Breast Implants on Breastfeeding. Plastic and Reconstructive Surgery.
- Cruz, N. I., & Korchin, L. (2010). Breastfeeding After Augmentation Mammaplasty with Saline Implants. Annals of Plastic Surgery, 64(5), 530–533.
- Semple, J. W. (2007). Breast-Feeding and Silicone Implants. Plastic and Reconstructive Surgery, 120(Supplement 1), 123S-128S.
- Vázquez, B., Ks, G., & Houston, G. C. (1987). Breast augmentation: A review of subglandular and submuscular implantation. Aesthetic Plastic Surgery, 11(1).
- Schiff, M., Algert, C. S., Ampt, A. J., Sywak, M., & Roberts, C. L. (2014). The impact of cosmetic breast implants on breastfeeding: a systematic review and meta-analysis. International Breastfeeding Journal, 9(1).
- Kappel, R. M., & Pruijn, G. J. M. (2020). Explantation of Silicone Breast Implants Ameliorates Gel Bleed Related Health Complaints in Women with Breast Implant Illness. Clinical Medical Reviews and Case Reports, 7(3).
- Ram, S., Ram, H. S., Rosenthal, Y. S., Attali, E., Warshaviak, M., Gamzu, R., Yogev, Y., & Chodick, G. (2021). The impact of breast augmentation on breast feeding in Primigravida Women – A cohort study. European Journal of Obstetrics & Gynecology and Reproductive Biology, 268, 116–120.
- Cruz, N. I., & Korchin, L. (2010b). Breastfeeding After Augmentation Mammaplasty with Saline Implants. Annals of Plastic Surgery, 64(5), 530–533.