How Soon Can I Spray Tan After Breast Implant Surgery
You can spray tan as soon as the incision heal completely. Tanning involves darkening the skin by increasing melanin production. After undergoing breast surgery, the next step involves incision scar recovery. However, any contamination of the incisions during recovery will affect the healing process.
Spray tanning after breast implant surgery does not affect the breast implants but can affect the skin and postsurgical scars. Scarring after breast augmentation is the body’s natural regeneration process to close the incision wound and enhance recovery.
So, is tanning safe? Should you spray tan after breast augmentation? Today, we’ll look at the best time to spray tan after breast implant surgery, when to start tanning, the effects, and everything related.
After How Long Can I Spray Tan After Breast Implant Surgery?

There are a few factors to consider regarding how long you should wait before you can spray tan. These include:
- Incision line/ scar maturation
- Wound healing
- Risks
You should protect yourself from sun exposure, bacteria and other skin infections, and dangerous chemicals that may impair healing.
“Patients should not spray tan on fresh incisions. A spray tan is recommended after successfully healing of the scars, usually after several months.” Says Dr. Beldholm. However, don’t assume the scars are ready for spray tanning without consulting your specialist surgeon. Applying spray tan too early after breast implant surgery will affect healing and worsen the scars. In addition, most scars are a different colour from the neighbouring skin, and spray tanning may cause them to appear more different and noticeable.
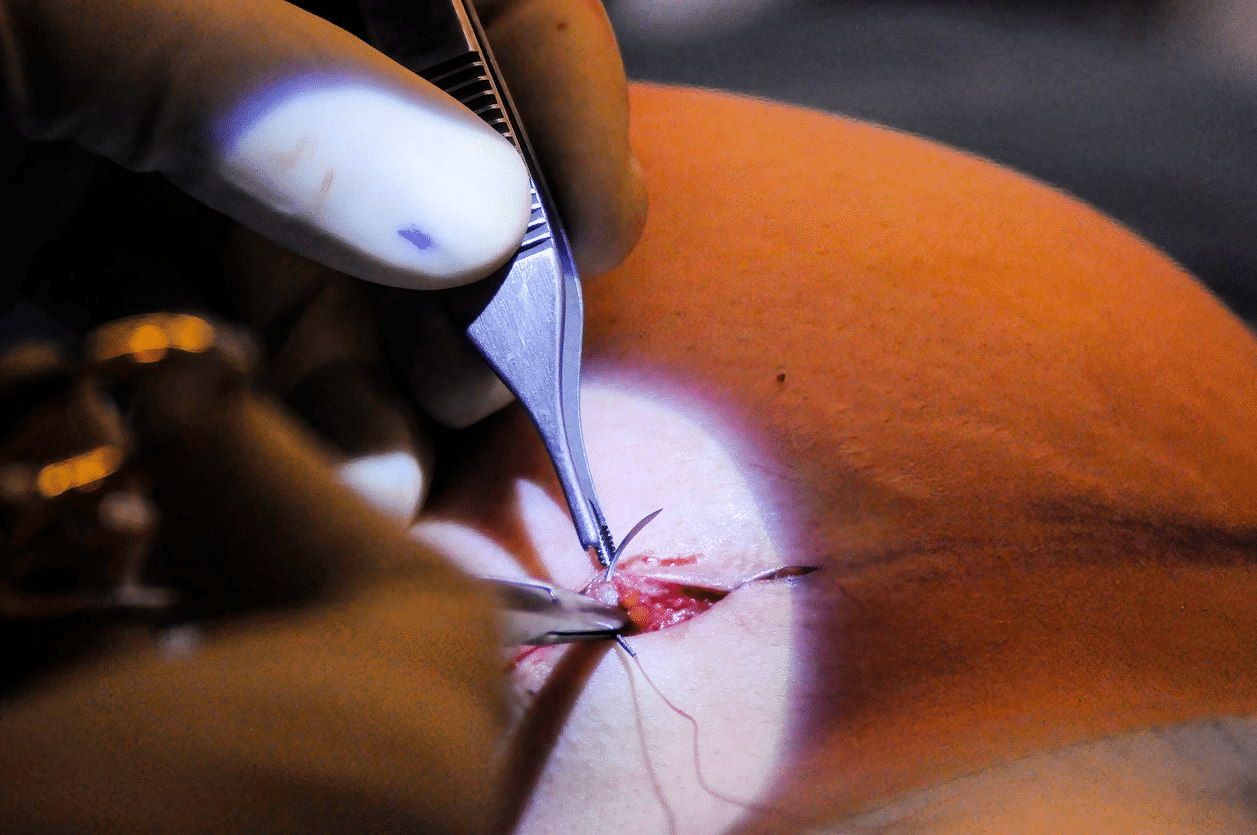
Understanding Breast Implant Surgery Postsurgical Scarring

Understanding how to use spray tan effectively is essential for postsurgical scarring. Below is the breast augmentation postsurgical scar recovery process.
Inflammatory Phase
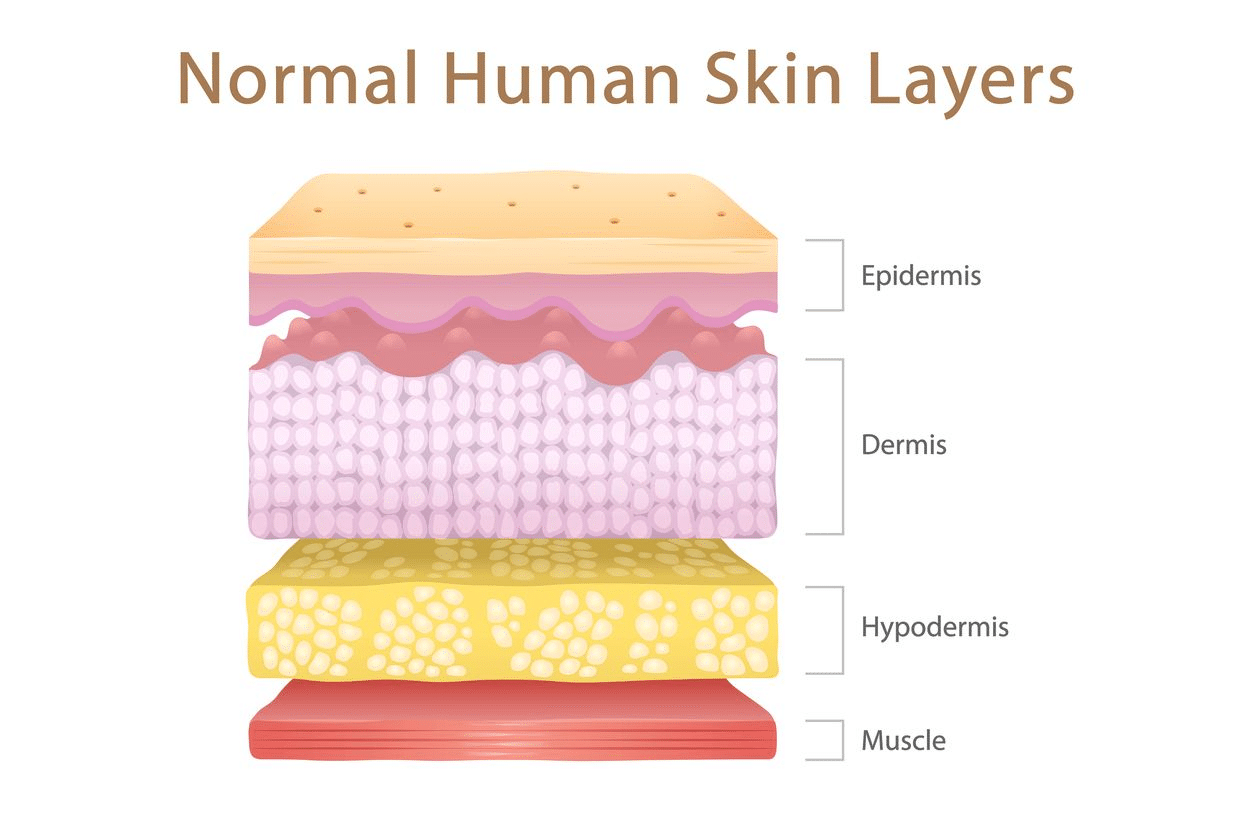
This is the first phase when the skin’s dermis (dermis is the thick and deep skin layer) gets injured. In response to the injury, the brain triggers the constriction of the blood vessels, reducing blood flow to the area and forming a clot.
The clot helps stop bleeding. After the bleeding ends, the blood vessels widen again, allowing white blood cells to pass through, fight any infections and repair the damaged tissue.
This process causes the wound area to swell, redden, and become warm and painful. After a few days, the incision wound becomes a dry and crusty scab, protecting the incisions.
Proliferation Phase
The second phase involves migration of the granulating tissue to the injured site to fill the wounds. In addition, the newly formed tissues start forming new blood vessels, supplying the skin cells with oxygen, essential nutrients and eliminating waste from the tissues. The last step in this phase involves the wound closing and the wound edges getting pulled together, resulting in a smaller wound.
Maturation Phase
The last phase begins many weeks after breast surgery and lasts longer. The wound matures, and the body starts thinning out unnecessary blood vessels and replacing them with newer collagen. The wound contraction continues as the injured tissue seals with collagen scar tissue. This causes the skin to become elevated and rough. The scar is unpleasant and can be excessive in some patients.
Full healing of the scar can take as long as 12 months. Patients considering excess scarring removal can consult a qualified surgeon after this phase.
The patient can use postsurgical scar treatment options like Fraxel Laser Treatment, CIT (Collagen Induction Therapy), silicone strips, and special ointment to enhance healing. However, Dr. Beldholm recommends using silicone gel strips and laser genesis. Skin needling can be done once the scar is more mature and if there are some raised areas.
Choosing a Spray Tan After Breast Augmentation

If you’re considering spray tanning, you must consider a few things and understand how to choose the proper spray tan. You can purchase spray tans from most beauty stores. Tanning products are available in liquid, cream, and spray, and have various fragrances.
When choosing a spray tan, the suitable option is to use a fragrance-free product because fragrant options may cause skin irritation. In addition, choose a natural mineral-based skin-tanning spray.
How to Maximise Spray Tanning Results
If you want to maximise the results of spray tanning, the first step is to avoid spraying the tan on fresh incisions and wait until the incisions are fully recovered. You should also thoroughly research spray tanning products before settling on one. You can consult specialised medical personnel on the issue. In addition, ensure you follow the pre- and post-tanning instructions from the doctor.
Before breast implant surgery, some pre-tanning instructions include avoiding tanning products at least 14 days before cosmetic surgery. This ensures the skin returns to its natural colour and has no extra bacteria and tanning chemicals that can cause infection. Also, you should exfoliate your skin to remove residual tanning products and avoid too much sun. Patients are also recommended to avoid harsh and scented exfoliating products.
When spray tanning, ensure you notify the spray tanning technician that you recently had a breast augmentation procedure. You may consider keeping the information private. However, notifying the technician will help them employ measures to protect the scars when spray tanning. They may also advise on what to do after spray tanning to ensure you’re comfortable during and after the process. Avoid spraying tan at all costs if you experience residual skin irritation or redness.
Are There Any Health Concerns Regarding Spray Tan?
There needs to be more research on the safety of spray tans. However, spray tans are not proven safe either. Spray tans consist of DHA or Dihydroxyacetone solution, ingredients used in skin darkening. The ingredients work on the skin’s dead cells, creating temporary skin darkening. This is what gives the skin a tanned appearance.
Some possible health concerns of the spray tan solution include:
- Contact dermatitis
- Vitamin D level disruption
- Eye irritation
- Skin damage
- Inhalation, which can affect the lungs
Additionally, the spray tan solution is not sterile and is moist. Therefore, spraying the solution on a fresh scar might be unhealthy and dangerous. Also, unwrapping and wrapping the dressed incision wound during spray tanning can cause skin irritation and breast implant malposition. Therefore, always consult your specialist surgeon if you want to spray tan after breast augmentation surgery.
Breast augmentation patients should avoid smoking, tanning, and other factors affecting scar healing after surgery.
What Other Tanning Options Are Available for You?

There are other different types of skin tanning methods. They include exposure to the sun’s ultraviolet rays and artificial tanning like tanning beds, sprays, and lotions. Tanning through exposure to the sun’s UVA rays is also known as natural tanning. Tanning sprays, creams, and lotions have temporary effects and are considered fake tanning. Let’s have a look at these tanning options.
Exposure to the Sun’s UV After Breast Augmentation: Should You Avoid It?
Although natural exposure to the sun is necessary for vitamin D, overexposure can be harmful. Exposure to the sun’s UV rays will affect scar healing and lead to darker scars. This is because scars don’t have any protective layer against the sun’s harmful UV exposure.
In addition, exposing the incisions to the sun during the first few days after surgery can increase postsurgical inflammation, worsening the swelling. To ensure uninterrupted recovery, you should avoid the sun for at least a week after surgery and limit its exposure afterwards.
Sun tanning can also increase the risk of hyperpigmentation, wrinkles, poor skin elasticity, and brown spots. In addition, sunbathing is associated with skin cancer.
To protect yourself from harmful UV rays, you should avoid prolonged exposure, wear protective clothing, avoid the sun’s peak hours, attend regular skin check-ups, and use sunscreens with sufficient SPF (Sun Protection Factor).
When Can I Get Sun Exposure After Breast Implant Surgery?
Unlike spray tanning, most doctors recommend avoiding sun tanning for more extended periods. The recommended time is 12 months after the incisions are completely healed. After this, you can go sunbathing but, ensure to protect your skin. However, the best advice is to avoid sun exposure or consult your surgeon before getting any sun exposure.
Using a Tanning Bed After Breast Augmentation

Sunbeds emit UV rays that tan the skin. There are no substantiated health benefits. These include boosting vitamin D levels attributable to exposure to artificial UV radiation in a solarium. Using sunbeds before complete scar healing will result in delayed healing and increased infection risk. In addition, it may have additional adverse effects like changes in thickness, colour, and appearance of the scar.
Ultraviolet rays from sunbeds also increase the rate of collagen breakdown and affect skin elasticity. Therefore, overexposure to these UV rays accelerates aging and increases the rate of breast sagging. Overexposure can also cause hyperpigmentation, sunburns, and dark spots.
Also, there are concerns that the UV rays from sunbeds can cause skin burns, increasing the risk of developing skin cancer. Research shows sunbed exposure increases the risk of melanoma and non-melanoma skin cancers. Melanoma is among the most complicated forms of skin cancer.
Commercial solariums are banned in all Australian states and territories except the Northern Territory, where no commercial tanning businesses exist. However, private ownership and personal use of solariums remain legal (and unregulated) in all states and territories.
Patients should note that sunbeds don’t enhance scar healing; but instead, they can negatively affect recovery. Therefore, breast augmentation patients should avoid sunbeds. If you must use a tanning bed after breast augmentation, you should protect the scars by covering them with a high-factor sun cream.
How Do You Prevent Postsurgical Scars Hyperpigmentation After Breast Surgery?
Normal surgical scars are hypopigmented after the maturation phase of scar healing. However, excess contact with UV rays after breast implant surgery leads to hyperpigmentation of scars.
Overexposure to UV rays is among the leading causes of hyperpigmentation after breast augmentation. Therefore, reducing exposure to sunlight can prevent hyperpigmentation of the healing scar wound. Also, you should wear protective clothing, like surgical bras, that limits the exposure of the scars and helps overall recovery. If you’re outside, use sunscreen to protect your skin and scars from the sun.
You should always protect your breast surgery scars from external elements that can negatively affect recovery. Avoid tanning sprays on surgical incisions because scars may reject the spray colour. In addition, you should avoid tanning beds.
Can You Self Tan Without Assistance from Tanning Personnel?
Yes! You can use self-tanning products, including creams, gels, and lotions. You can also self-tan using tanning sprays. However, it’s essential to follow the tanning instructions on the products.
Final Take
Tanning after breast implant surgery does not affect the breast implants but can affect the skin and postsurgical scars. Spray tans can negatively affect scar healing and increase the risk of additional breast implant-related infections. Surgeons recommend avoiding spray tans and only using them after the incisions have healed completely. Spraying tan on the incision lines before full recovery can cause the scars to reject the spray, causing them to have a different colour from the rest of the skin.
In addition, patients should also avoid other tanning methods like the sun and sunbeds. Overexposure to UV rays from these tanning methods can affect scar healing and cause hyperpigmentation and skin cancer. Note that tanning beds are banned in Australia. The key is to consult a specialist surgeon before spraying, sun, or sunbed tanning.
References
- Everaars, K. E., Welbie, M., Hummelink, S., Tjin, E. P., De Laat, E. H., & Ulrich, D. (2020). The impact of scars on health-related quality of life after breast surgery: a qualitative exploration. Journal of Cancer Survivorship, 15(2), 224–233.
- Barrington, M. J., Seah, G. J., Gotmaker, R., Lim, D., & Byrne, K. (2020b). Quality of recovery after breast surgery. Anesthesia & Analgesia, 130(6), 1559–1567.
- Peng, G. L., & Kerolus, J. L. (2019). Management of surgical scars. Facial Plastic Surgery Clinics of North America, 27(4), 513–517.
- Son, D., & Harijan, A. (2014). Overview of surgical scar prevention and management. Journal of Korean Medical Science, 29(6), 751.
- Madigan, L. M., & Lim, H. W. (2016). Tanning beds: Impact on health, and recent regulations. Clinics in Dermatology, 34(5), 640–648.
- Bowers, J. M., Geller, A. C., Schofield, E., Li, Y., & Hay, J. L. (2020). Indoor tanning trends among US adults, 2007–2018. American Journal of Public Health, 110(6), 823–828.
- Choi, K., Lazovich, D., Southwell, B., Forster, J. L., Rolnick, S. J., & Jackson, J. (2010). Prevalence and characteristics of indoor tanning use among men and women in the United States. Archives of Dermatology, 146(12), 1356.
- Kwon, S. H., Barrera, J. A., Noishiki, C., Chen, K., Henn, D., Sheckter, C. C., & Gurtner, G. C. (2020). Current and emerging Topical scar mitigation therapies for craniofacial burn wound healing. Frontiers in Physiology, 11.
- Garg, S., Weissman, J. P., Reddy, N. K., Varghese, J., Ellis, M. F., Kim, J. Y., & Galiano, R. D. (2022). Patient-reported outcomes of scar impact: comparing of abdominoplasty, breast surgery, and facial surgery patients. Plastic and Reconstructive Surgery. Global Open, 10(10), e4574.
- Sidgwick, G. P., McGeorge, D., & Bayat, A. (2015). A comprehensive evidence-based review on the role of topicals and dressings in the management of skin scarring. Archives of Dermatological Research, 307(6), 461–477.