How to Choose the Right Breast Implant Type for Breast Reconstruction
Undertaking a breast augmentation is a decision that requires some deep thought. For many women, this is when they want to restore the breasts they had and feel empowered. Making such a decision is one step, but choosing the right type of breast reconstruction is another major one.
Women might choose to undergo surgery after surviving breast cancer. However, the decision is personal. This is why you’ll often come across this question “What is the best breast implant size and type for breast reconstruction?”
We’re here to help. Today we bring you tips and tricks to help you choose the right breast implants Newcastle for yourself.
Breast reconstruction after mastectomy

A mastectomy is a procedure that involves the removal of all breast tissue from a breast to prevent or treat breast cancer. This Surgery can be done in one breast “unilateral” or both breasts “bilateral.”
Breast cancer usually occurs in one breast only. If a patient is diagnosed with breast cancer, they may require either a lumpectomy or mastectomy. Mastectomy involves removing the breast tissue, which can result in significant breast asymmetry. Ideally, one side will have no breast tissue, while the other will have the patient’s normal breast.
Where mastectomy is necessary, the patient may choose to have breast reconstruction surgery to rebuild the breast to match breast shape on the other side. However, the reconstructed breast will typically be more perky than the natural breast. This is because it may be saggy. As a result, the patient may require a breast lift or reduction to achieve a more symmetrical appearance. This process may require several operations to get the best possible outcome.
Having mastectomy done on both sides is less common. However, if patients test positive for BRCA genes, they may choose to have bilateral mastectomies to reduce the risk of breast cancer. The patient needs to see a multidisciplinary team or a breast cancer surgeon to help them make an informed decision.
If a patient has bilateral mastectomies, there are several options for breast reconstruction. One option is to have bilateral breast implants. However, the surgeon should consider the size and shape of the breasts that best suit the patient. The reconstruction process may, however, require multiple surgeries to achieve the desired result.
Radiation treatment to chest wall
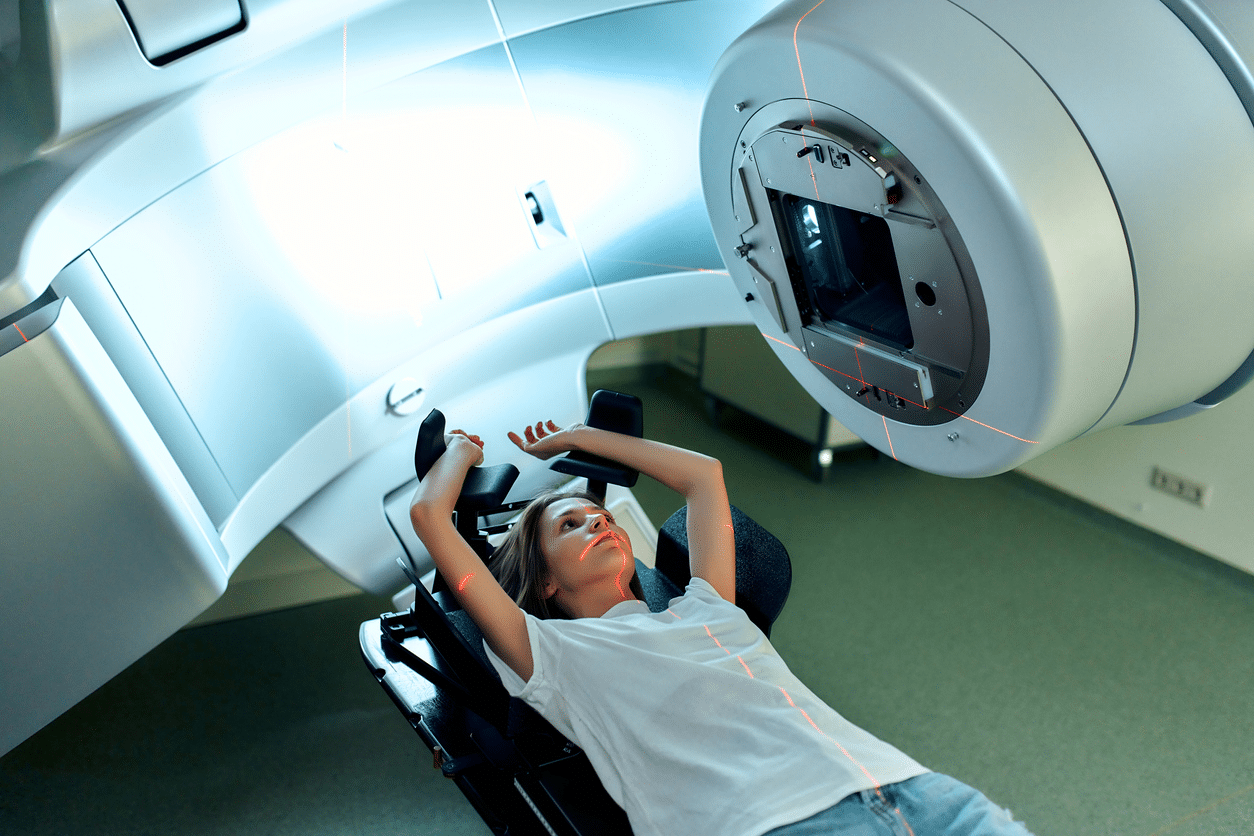
Radiation therapy is a treatment used to treat breast cancer. It uses high-energy radiation to destroy cancer cells. While the procedure works well on most breast cancer patients, it is more likely to damage the surrounding healthy tissues. The most affected parts include;
- The skin
- Muscles
- Bones
- Chest wall
The changes caused to the chest wall and skin makes it less pliable and prone to complications during breast implant reconstruction. How?
- Skin Damage: Radiation might damage the skin and the surrounding tissues. This makes it less able to stretch or accommodate an implant increasing the complication risks such as poor wound healing.
- Increased risk of infection. Radiation can affect the immune system making it difficult to fight infection. This might lead to risks such as implant exposure.
- Fibrosis: Radiation causes thickening of the chest wall tissues. This makes it hard for a surgeon to create an implant pocket. It also increases the risk of capsular contracture, where scar tissue forms around the implant, causing it to deform or harden.
Breast implants may not be ideal for women who have undergone radiation therapy. Instead, the surgeon may recommend other options, like autologous tissue reconstruction. Patients should note that each case is unique, and one should evaluate and consult with the surgeon before deciding.
Breast Reconstruction Options
Breast reconstruction can be divided into Autologous (using tissue from the patient’s body) and implant-based reconstruction.
Autologous Reconstruction
This type of breast reconstruction involves using tissues from other parts of the patient body, such as the abdomen, buttocks, or back, to create a new breast. The tissue can be used in different ways, including as a free flap or pedicled flap.
A free flap is where the tissue is completely detached from its original blood supply and reconnected to blood vessels in the chest. On the other hand, pedicled flap, the tissue remains attached to its initial blood supply and passes under the skin to the chest.
It’s important to note that autologous reconstruction is more complex than breast implant-based reconstruction and may require more recovery time. Furthermore, since it involves surgery on different body parts, it can result in additional scarring and recovery time.
Breast Implant-Based Reconstruction
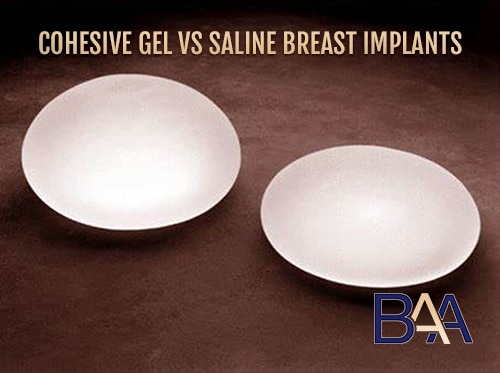
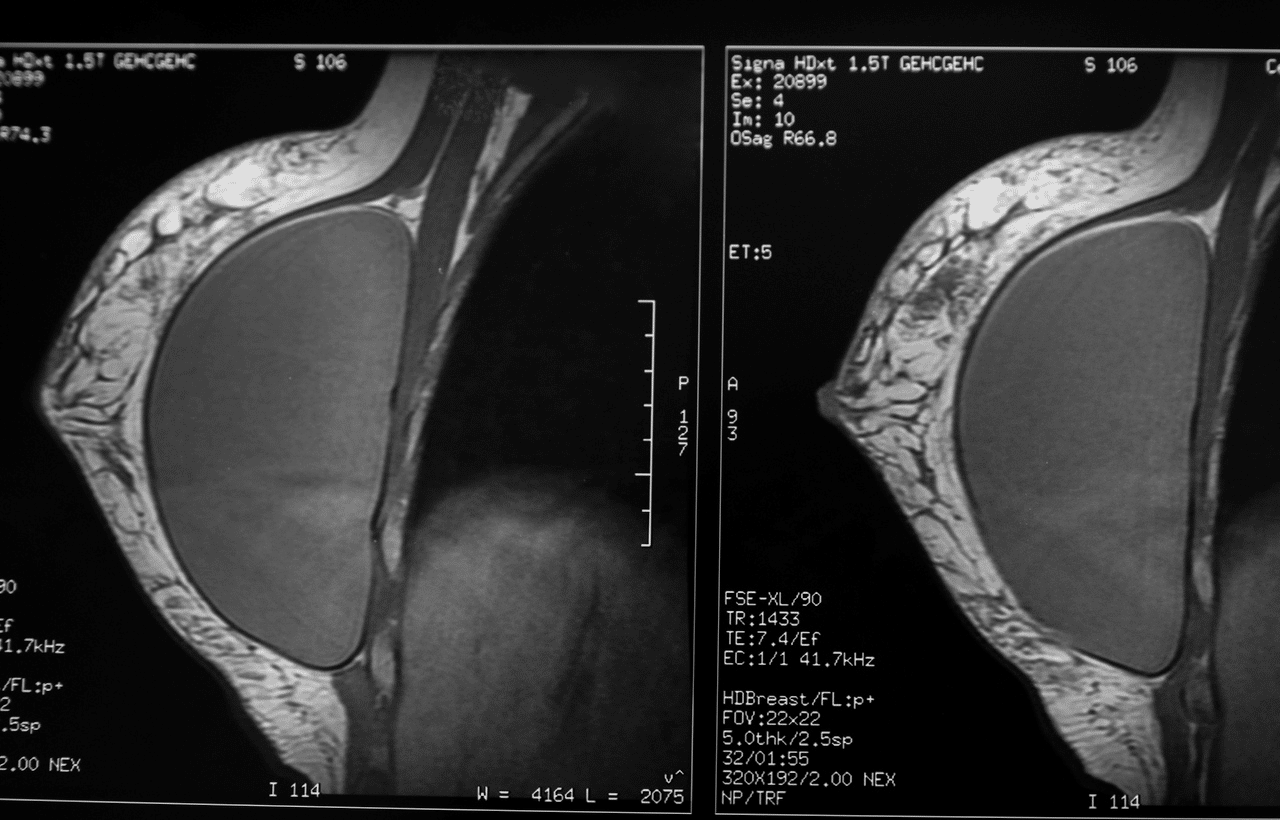
Implant-based reconstruction involves using a breast implant to create a new breast. This can be done using either a silicone or saline implant. The silicone implant can be placed under the chest muscle or directly behind the breast tissue.
There are also hybrid techniques that combine both autologous tissue and implants. For instance, a surgeon might use a flap of tissue from the abdomen to create the shape of the breast and then place an implant behind it to add volume.
The choice of reconstruction method depends on various factors. These include:
- Patient anatomy
- The cancer stage
- Patient personal preference.
It is, therefore, important to discuss all the available options with your healthcare team to determine which approach suits you best.
What are the Pros & Cons of Breast implant vs autologous
Breast Implants
Pros
- Allow customisable shape and size. Breast implants come in various shapes and sizes. This allows for more customisable options based on the patient’s body type and preference.
- Less invasive. Since breast implant surgery is less invasive, there is less scarring, and the patient can serve a shorter recovery period than autologous.
- Immediate results. The results of breast implants are usually noticeable exactly after the procedure.
- Less surgical scars. Breast implant results in fewer scars as compared to autologous reconstruction.
Cons
- Complication risk. Some major risks of breast implants are; implant rupture, capsular contracture, and infection.
- Need for additional surgery. Breast implants are not permanent; therefore, they may need to be replaced or removed sometime in the future.
Autologous Breast Reconstruction
Pros
- Uses natural tissues. There is a more natural look and feel since autologous breast reconstruction uses the patient’s own tissue to reconstruct the breast.
- Long-lasting results. The results are long-lasting; since the reconstructed breast tissue is a permanent part of the patient’s body.
- Less risk of implant-related complications. Since Autologous does not involve the use of implants, there is less risk of implant-related complications such as rapture.
- High Potential for improved symmetry. Surgeons can use autologous to enhance the balance between two breasts. This may not be possible with breast implants alone.
Cons
- Longer recovery time. This process is more invasive than breast implant surgery. For that reason, it calls for a longer recovery time.
- Scaring risk. Autologous involves several incisions leaving scars on both the donor part and the breast.
- Limited availability. Not all patients qualify for autologous breast implants. This is because the process requires sufficient healthy tissues to complete the procedure.
Breast Implant reconstruction
Several types of breast Implant reconstructions are available to women who have undergone a mastectomy or lumpectomy. This method involves using saline and silicone implants to recreate the size and shape of the breast.
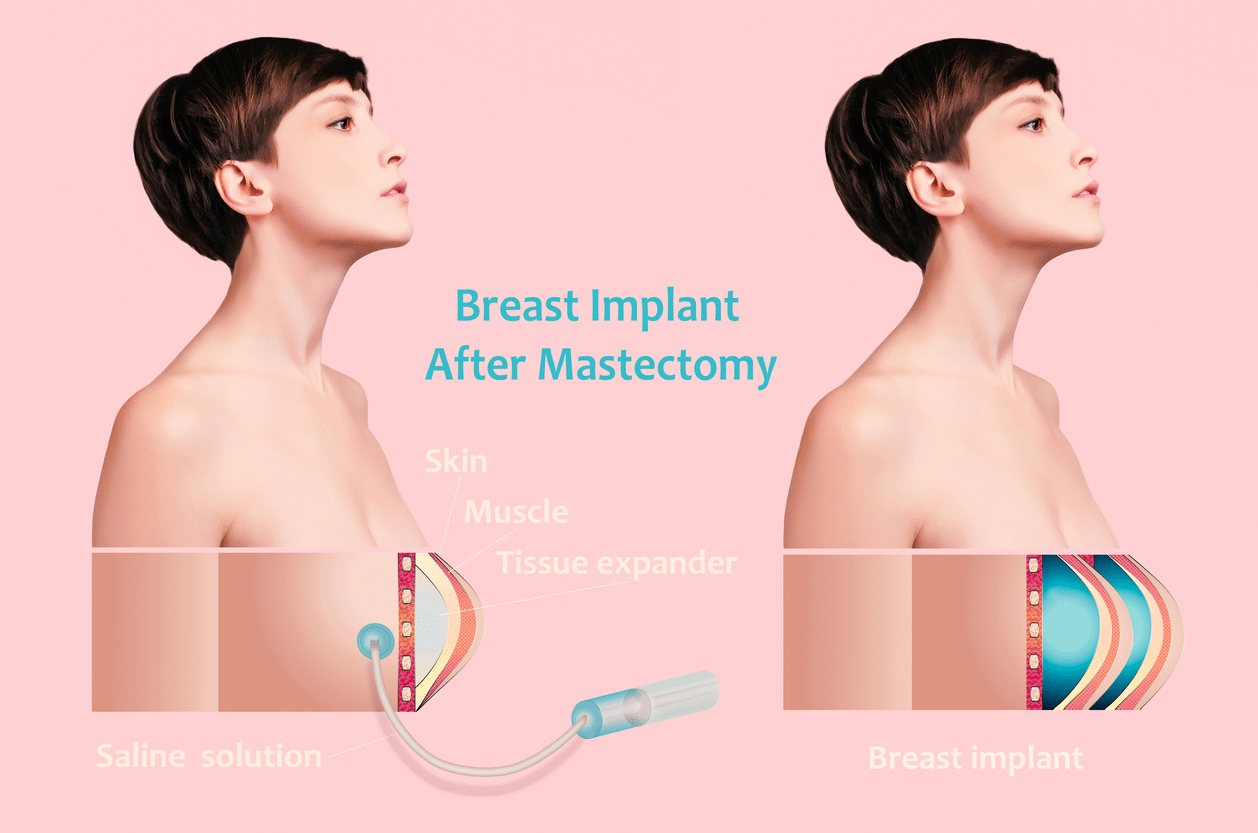
Staged breast reconstruction
This involves initially inserting an expander under the chest muscle to stretch the skin and create a natural breast shape and implant pocket. It is an ideal technique for women who have undergone a mastectomy and want to restore the shape and size of their breasts.
During the mastectomy surgery, the staged breast reconstruction process typically begins with placing a tissue expander under the chest muscle. The tissue expander is removed and a permanent breast implant is inserted in its place once the skin has been suitably stretched. The final permanent implant used can be either saline or silicone; the patient can choose it based on their medical history and preference.
Recovery from the second stage of the surgery may take several weeks. Patients may experience discomfort, swelling, or bruising during this time. The surgeon will provide detailed instructions for post-operative care and follow-up appointments to ensure proper healing.
This type of breast implant comes with various benefits. Ideally, by stretching the skin over time, the final results appear less stressed and natural. Additionally, the approach can reduce the risk of complications such as infection or implant displacement when the implant is placed immediately after the mastectomy flap reconstruction surgery.
Patients need to note that it’s essential for patients to note that staged breast reconstruction is a process that can take several months to complete. At some point, it may require multiple surgeries. Patients should also be aware of the potential risk and complications associated with the procedure. They should also discuss with their surgeon before undergoing the procedure.
One stage breast reconstruction
This is where the surgeon performs a mastectomy, usually nipple-sparing and then inserts a breast implant as part of the same operation. It is common in women diagnosed with breast cancer who require mastectomy to remove the cancerous tissue.
The one stage breast reconstruction technique is typically done using a nipple-sparing mastectomy approach. The surgeon will make a small incision around the nipple and remove the breast tissue through this opening.
Once the breast tissues are removed, the surgeon will insert a breast implant and position it in place through the same incision. This means that the nipple and the areola are preserved during the mastectomy surgery, providing more natural-looking results after reconstruction.
Some of the benefits of one-stage breast construction include the following;
- Shorter overall treatment time
- More looking natural results
- Reduced emotional stress
Unlike staged reconstruction, the patient doesn’t need to undergo a second surgery since the reconstruction is done as part of the same operation as the mastectomy.
As with any surgical procedure, there are risks associated with one-stage breast reconstruction. The patient may experience bleeding, infection, or other complications during or after surgery.
What To Consider When Choosing Breast Implants?
Since many implants exist today, choosing the most appropriate type can be overwhelming. This is why it is essential to have a transparent one-on-one consultation with a surgeon before undertaking the surgery. It’s also ideal for the patient to have a second opinion to get more insight if they are comfortable.
Why so? Implant selection is individualized since similar implants in two patients might look very different. Therefore, here are a few factors to guide you when choosing the right breast implant placement type for breast reconstruction.
What Size Are You Looking For?
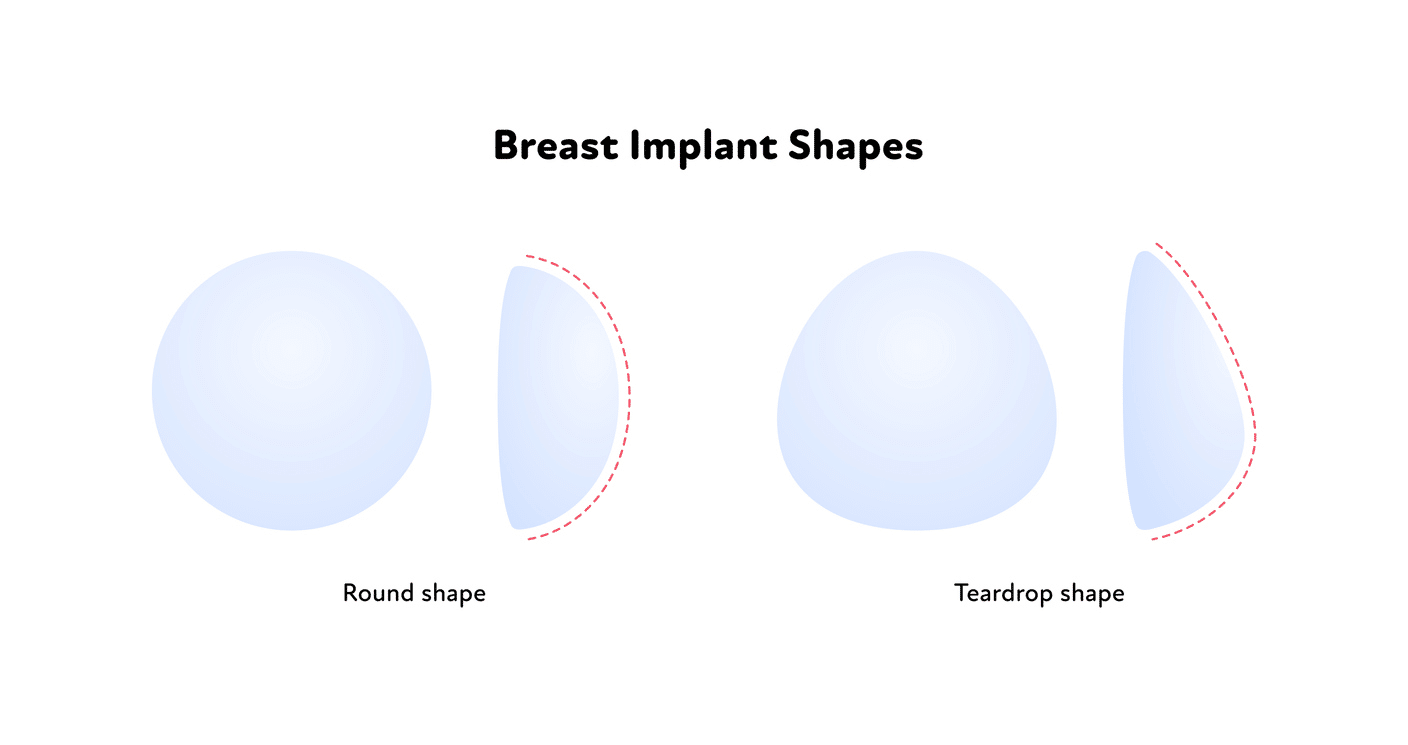
Both the saline implants and silicone come in various sizes and shapes. Chances are, your surgeon will ask you, “What size do you prefer?” during your consultation visit. Most patients usually know the size they want, but thinking more about this is essential. The implant size depends on various factors such as:
- Size and shape of your chest
- Lifestyle
- Personal Aesthetic goals
In addition to choosing an implant that works best with your body type, selecting an implant size that fits within the boundaries of safety and health is crucial. Patients should also go for something that complements their body type.
Coverage of the Soft Tissue
When choosing the right breast augmentation, it is ideal to consider your skin’s laxity and the thickness of the soft tissue. This is determined by the soft tissue pinch test carried out at the upper medial pole of the patient’s breast.
Once you understand your soft natural breast tissue thickness, you can choose a more or less cohesive implant. It’s important to note that one should not confuse skin viability and quality with soft tissue thickness.
A more cohesive implant may be ideal if the patient has thin, soft tissue coverage. This will prevent rippling or implant visibility. Conversely, a surgeon may use a less cohesive implant for soft but thick tissue patients to provide a more natural feel of the reconstructed breast.
Proportion
Here is another essential factor to consider. To look “natural,” the shape and size of your implants should perfectly fit the dimensions and contours of your body. During your consultation visits, your surgeon will take your rib cage, chest wall, and fat pad measurement.
This will help to determine the size that fits best. In addition to breast implant sizes, different types of breast implants for breast reconstruction may have varying degrees of projection. This includes the height and the width, which can affect the final results. It is, therefore, essential to consider this before deciding on the kind of breast implant you want.
Appropriate Surgical Technique
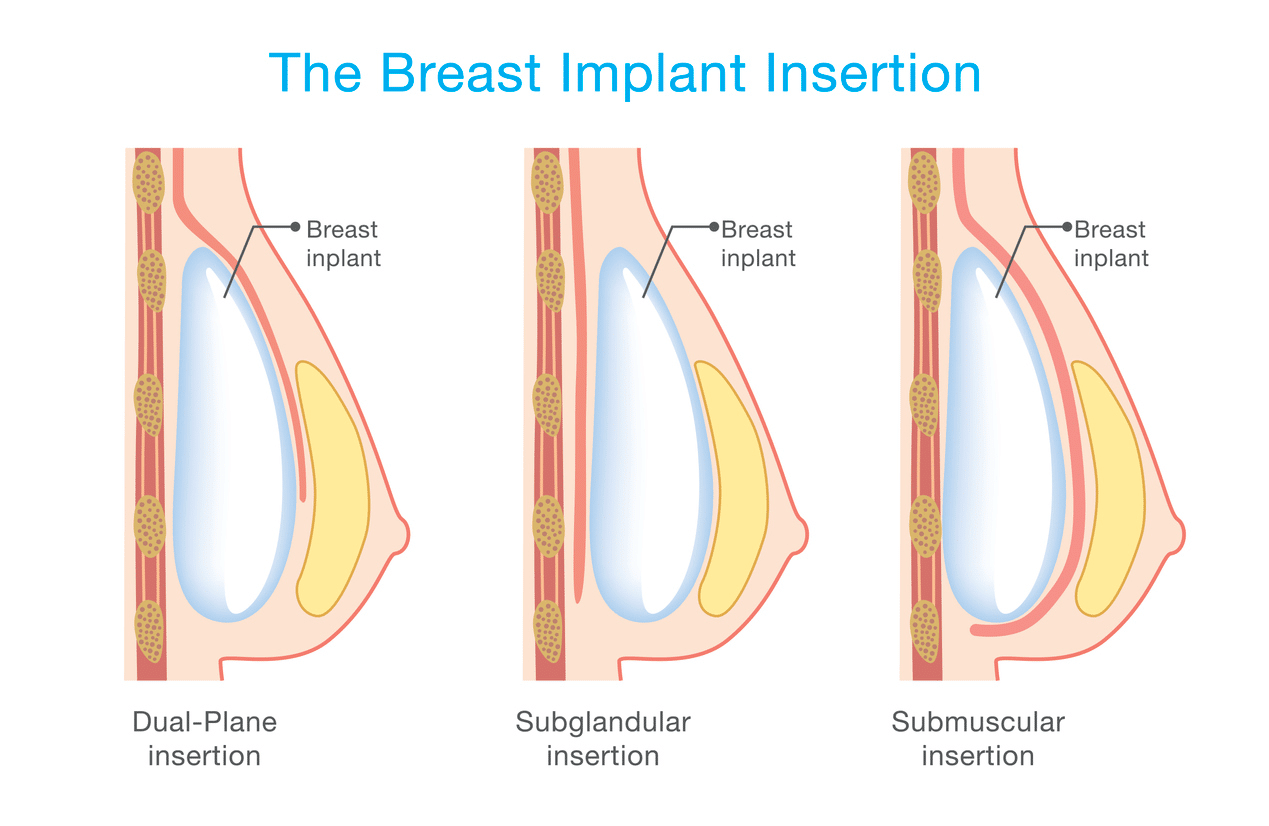
Various textures come with breast implants. These include smooth and textured, and each type offers different benefits. Smooth implants move more naturally with the body.
Choosing an appropriate surgical technique is as important as picking the right breast implant size and type. When considering breast augmentation in Sydney, you should know that the technique used by your surgeon will determine the implant’s position and shape.
That said, it is vital to consider a surgeon who has experience with various surgical techniques. An experienced surgeon can provide personalized recommendations based on patient needs.
Remember, some factors will determine the ideal surgical technique for you. These include:
- Patient anatomy
- Amount of breast tissue
- Location of incision
Personal Preference
Individual preference is another worth noting factor. As far as you’re considering the above points, it’s ideal to consider personal desire.
It is essential to consider how you need your reconstructed breasts to feel and look. Consider the type that will fit your body perfectly and give you the desired appearance. Would you love breast implants that are pre-filled with silicone gel or saline? What about those filled when inserted into the chest walls?
Each of these kinds has its benefits and disadvantages. This is why it is essential to discuss with your surgeon before deciding. Let them know if you have any specified desire for texture or other aesthetic concerns. Also, as aforementioned, the appearance/result of the implant might be different from one patient to another.
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) is a rare form of cancer associated with breast implants. It develops in the scar tissue and fluid surrounding the breast implant. It’s ideal to note that this is not a breast cancer.
This rare type of cancer is estimated to occur in approximately 1 in 3,817 to 1 in 30,000 women with textured breast implants. However, this will depend on the type of implant and other various factors. The risk of developing this type of cancer is lower for women with smooth implants. This means most women with breast implants have a higher chance of not developing it.
Symptoms of BIA-ALCL include;
- Swelling
- Pain in the breast or armpit
- Lumps
- Redness or skin rash around the breast
Asymmetry in breast or armpit might develop several years after breast implant surgery. Sometimes, the patient might experience systematic symptoms such as fever, fatigue, or night sweats. If a patient experience these symptoms, they should contact the healthcare provider immediately.
BIA-ALCL is related to an immune response to the textured surface of some breast implants, which can trigger the development of lymphoma cells in the surrounding tissue.
Treatment for BIA-ACLC involves the removal of the breast implant and the surrounding scar tissue. In some cases, additional treatment, such as chemotherapy or radiation therapy, may also be necessary. The prognosis for BIA-ALCL is generally reasonable, particularly if the cancer is caught early and treated promptly.
The TGA recommends that women with breast implants monitor their breast changes to reduce the risk of BIA-ALCL. If they experience any symptoms, the patients should not hesitate to contact their healthcare provider immediately. Women with breast implants should also undergo regular checkups with their plastic surgeon or healthcare provider.
In October 2019, Australia banned three-highly textured breast implants since they were highly associated with BIA-ALCL. However, microtextured and smooth breasts are considered safe, so they remain available.
As Dr. Bernard Beldholm says, “It’s important for women with breast implants to stay informed about the current recommendations and developments regarding breast implant safety.”
Patients should note that breast implant is a broad topic that has been extensively studied. Well, as much as they are considered safe, there are potential risks, similar to any other medical procedures. This is why they should stay up to date and discuss with their healthcare provider before making the final decision.
You Don’t Know Where to Start? We Can Help
If you’re considering undertaking a breast implant augmentation in Sydney and don’t know where to start, a breast augmentation Australia surgery clinic can help. Dr Bernard is ready to help you achieve your aesthetic goals. Book a consultation to learn more about breast implants before deciding.
References:
- https://www.plasticsurgery.org/patient-safety/breast-implant-safety/bia-alcl-summary
- https://www.fda.gov/medical-devices/breast-implants/questions-and-answers-about-breast-implant-associated-anaplastic-large-cell-lymphoma-bia-alcl
- https://www.smh.com.au/national/three-highly-textured-breast-implants-banned-over-cancer-fears-20201030-p56a1c.html
- Three highly textured breast implants banned over cancer fears (smh.com.au)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma in Australia: A Longitudinal Study of Implant and Other Related Risk Factors – PubMed (nih.gov)
- BIA-ALCL: Information for health professionals | Therapeutic Goods Administration (TGA)