Breast Implant Capsular Contracture
Capsular contracture happens when the tissue surrounding breast implants hardens and squeezes the implant. This distorts the breast shape, causing chronic pain and discomfort. Capsular contracture is the main breast-implant related complication with an overall incidence of 10.6%, and a major reason for reoperation.
When the surgeon inserts the breast implant into the breast pocket, scar tissue forms around the implant. The formation of the fibrous capsule is the body’s natural reaction to any foreign material. The scar tissue is normally soft and unnoticeable, and it’s part of healing. The capsule helps hold the implant in place, preventing rotation or malposition. However, there are cases when the fibrous capsule hardens and starts contracting, leading to capsular contracture.
Stages Of Capsular Contracture
Baker classification for capsular contracture | BAA
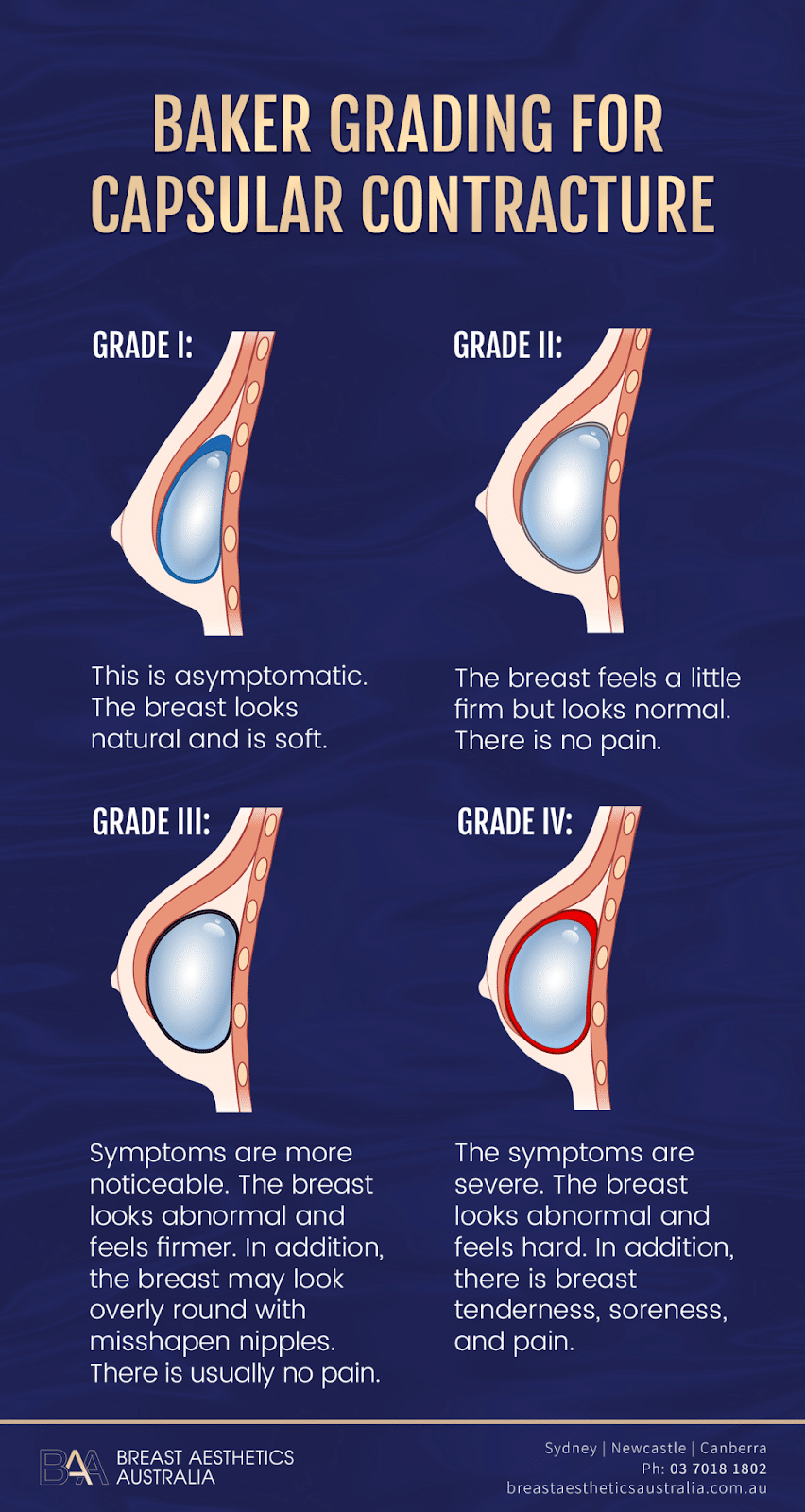
Different degrees of capsular contracture are rated using the four-grade Baker scale.
- Grade One: The first stage shows little or no symptoms (asymptomatic). The scar tissue doesn’t affect the breast shape, size, or texture. The breast looks and feel normal.
- Grade Two: At this stage, minor symptoms start showing. The breast shape remains normal, but they feel firm on touch.
- Grade Three: The breast appearance changes. The shape looks abnormal, overly round, and hard looking, with misshapen nipples. They also feel hard on touch. However, there’s little or no pain at this stage.
- Grade Four: Like stage three, the breast is hard and distorted. In addition, the patient experiences breast tenderness accompanied by pain on touch. Grade iv capsular contracture is severe and requires medical attention.
Causes of Capsular Contracture
The main explanation for the cause of Capsular Contracture is the body protecting itself from the breast implant (a foreign material) and forming scar tissue. However, there’s no complete understanding of the cause of capsular contracture. This is due to insufficient information about the complication and the fact that only a small number of women get the complication. Some proposed theories by researchers and medical practitioners to explain the complication include:
Immunologic Response
During the healing process after breast augmentation, the body creates a fibrous capsule. This is a body’s immune system reaction intended to surround and isolate the breast implant from the rest of the breast tissue. It also helps the implant’s position, preventing implant rotation.
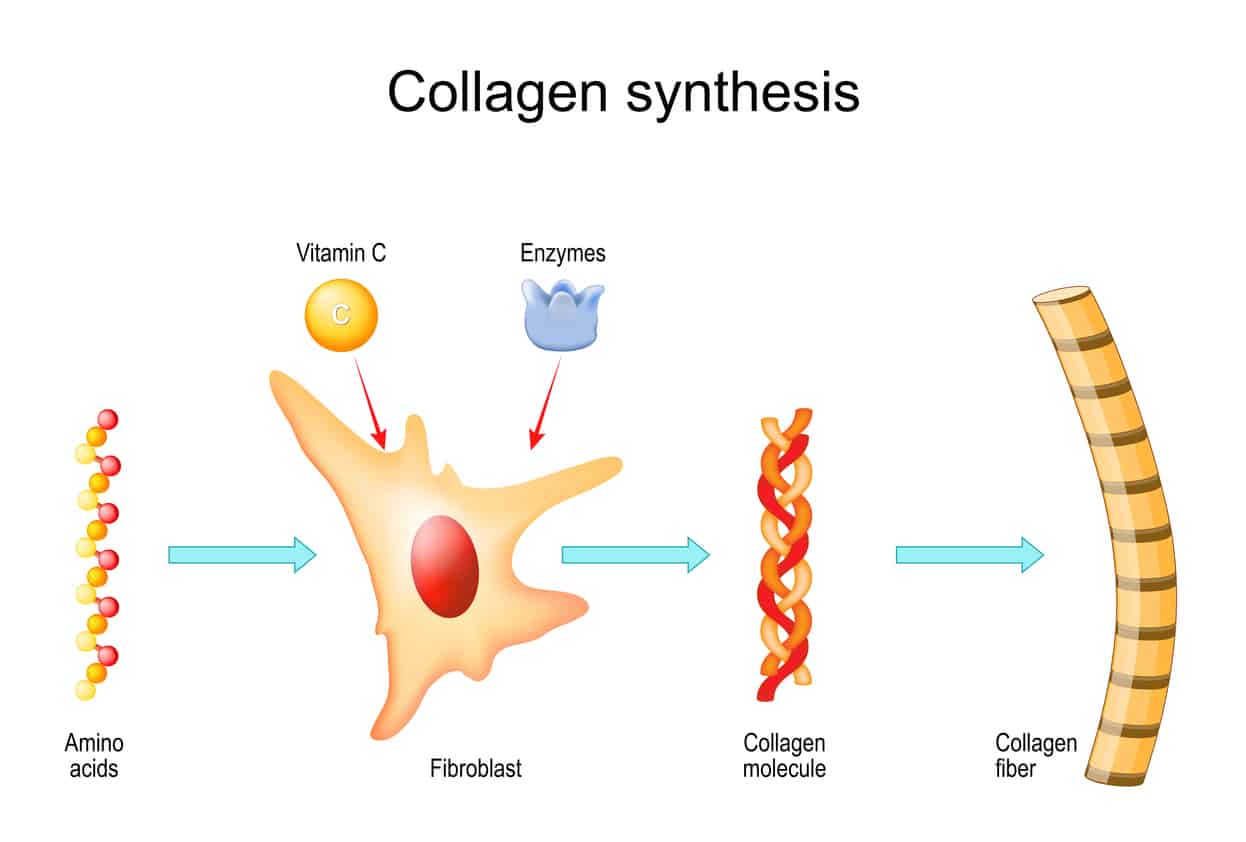
This is a normal immune response process. However, some patients may have an excess immune response prompting the body to develop a thicker capsule of more rigid, large fibrous bands, causing capsular contracture. The capsule’s cellular composition is mainly fibroblasts, lymphocytes, and macrophages. The implant and the capsule contact zone have an increased accumulation of fibroblasts.
Studies of capsular tissue shows that the majority of the tissue contains uniformly distributed collagen fibres. Their organisation and orientation of the collagen fibres change as contracture severity worsens. The fibres thicken and appear as cable-like bundles. Other agents like interleukins and the connective tissue growth factor promote fibrosis.
In addition, the study shows that myofibroblasts, which are contractile fibroblasts, provide a contractile force, decreasing the surface area of the capsule. This aids the collagen matrix to remodel and stabilise the contracture.
Inflammatory Reaction

Some surgeons believe that bacterial contamination of the breast implant may lead to adverse inflammation of the breast tissue. Bacterial contamination creates a biofilm on the implant’s surface, causing a low-grade infection. As the body fights the infection, it may cause inflammation, forming a thicker fibrous capsule.
The bacteria results from contact between the breast implant, the patient’s skin, or any other external materials. The Staph bacteria are the main bacteria associated with the infection, found on the skin and the nipple, with the Staphylococcus epidermidis species may play a huge role. It increases capsule pressure and leads to a thicker capsule with increased collagen density and angiogenesis, associated with capsular contracture.
However, medical researchers disagree on the validity of this theory on its role in causing capsular contracture.
Seroma and Haematoma
The theory suggests that excess bleeding and fluid pooling around the breast implant can cause capsular contracture. Accumulation of blood around the implant results from trauma, damage of the blood vessels, or use of certain medications, among other factors.
The fluid and blood feed the bacterial biofilm that forms on the breast implant with nutrients, encouraging growth. Growth of the bacterial biofilm increases the risk of complications.
Genetic Predisposition

Some women have a higher risk of developing capsular contracture than others due to their genetics. Patients whose family has a history of autoimmune disease or thick scar tissue face a higher risk of capsular contracture.
However, it’s hard to predict accurately if a patient will develop capsular contracture. Therefore, breast surgery patients should notify the surgeon of their medical history to help apply measures to reduce capsular contracture occurrence.
Breast Reconstruction After Breast Cancer
Patients who undergo reconstructive breast surgery after breast cancer treatment are more susceptible to capsular contracture. Chemotherapy and radiotherapy are known to increase the formation of fibrous capsules.
Signs and Symptoms of Capsular Contracture
Capsular contracture can be hard to notice in the early stages. However, the signs and symptoms are easily visible in the third and fourth stages. A patient should seek immediate medical attention if they notice any breast abnormality. The common symptoms of capsular contracture include:
- Breast tenderness
- Hardness around the breast implant
- Tightness around the chest muscles
- Rippling
- Breasts abnormally round
- Pain (this signifies the complication is severe)
Diagnosis of Capsular Contracture

When a patient experiences any capsular contracture-related symptoms, the surgeon will recommend one or more tests to ascertain. Before performing any tests, the surgeon will assess the degree of firmness, deformity, tenderness, and pain. Some of the tests for capsular contracture diagnosis include:
- Mammography: The test helps detect moderate and mild capsular contracture. However, its usage is restricted in cases of severe capsular contracture. Mammograms are common in detecting breast cancer.
- MRI Scan: Magnetic Resonance Imaging is one of the top methods used in capsular contracture diagnosis and other breast-related complications. The test produces high-quality imaging of the breast implant and tissue, enhancing the test’s quality. Capsular contracture leads to an increased number of radio folds.
- Ultrasound: This is another detection method. However, in detecting capsular contracture, the quality of the ultrasound test depends on the doctor’s experience. This may be a setback.
Surgical Treatments of Capsular Contracture

Revision surgery is the standard surgical treatment of capsular contracture. This involves the removal of the implant and capsule and the replacement of the breast implant. The treatment is suitable for patients with grade iii or iv capsular contracture. However, surgical treatment of capsular contracture is associated with about 25% recurrence rate of capsular contracture in the first year.
Below are some of the surgical techniques used in the treatment of capsular contracture:
Capsulectomy
This revision surgery technique involves the removal of the whole scar tissue surrounding the breast implant. It’s more invasive than Capsulotomy and involves higher risk. Patients with submuscular implant placement face a higher risk of haematoma or pneumothorax after capsulectomy.
However, some surgeons and patients prefer this technique because it ensures the removal of all the contaminants and reduces the risk of further contracture. In addition, capsulectomy prevents calcium buildup in the remaining breast tissue and reduces the interference of a mammography test. In most cases, the surgeon usually performs a capsulectomy and a site change for the new implant.
Capsulotomy
A Capsulotomy is a surgical technique where the surgeon tries to free the breast implant by removing capsule sections. The surgeon makes the incisions to loosen the implant in different orientations and locations.
This helps restore the breast’s appearance without entirely removing the capsule. A Capsulotomy is suitable if the primary breast augmentation uses submuscular placement. It is less extensive and risky compared to capsulectomy. This method is also known as open Capsulotomy.
Fat Grafting
Autologous fat transfer involves using liposuction to harvest fat from body parts like the thighs, buttocks, or abdomen and injecting it into the breasts. Researchers note that the technique enhances blood circulation around the capsule preventing capsular contracture. However, insufficient evidence fully supports this method in treating capsular contracture.
Breast Implant Replacement
This prosthetic breast reconstruction involves removing and replacing the implant with a new one. In this technique, the surgeon creates a new breast pocket for the breast implant. This reduces the reoccurrence of the complication. Most surgeons incorporate the technique with capsulectomy and Capsulotomy to improve the results.
Implant Removal Without Replacement
Complete removal of the breast implant helps treat and prevent the reoccurrence of capsular contracture. However, this may affect the breasts’ aesthetics and lead to breast ptosis (sagging). The surgeon may suggest breast lift (mastopexy), autologous fat transfer, or excess skin removal to reduce breast ptosis.
Nonsurgical Treatments of Capsular Contracture
Although most plastic surgeons conduct surgical treatment of capsular contracture, there are nonsurgical methods to consider as well. Below are some of the nonsurgical capsular contracture treatment methods.
- Ultrasound Therapy– It involves using sound waves to soften the scar tissue.
- Closed Capsulotomy– This involves breaking the scar tissue without surgery. This technique is not fully effective and has a high risk of causing haematoma and implant rupture.
- Injectables– Some medications like Triamcinolone and Botulinum toxin are injected into the scar tissue to make it softer and thinner
- Oral Medications– Researchers propose using oral medications like Montelukast, Zafirlukast, and Pirfenidone in capsular contracture treatment.
How to Reduce/ Prevent Capsular Contracture
Here are a few practices that one can use to prevent Capsular Contracture.
Submuscular placement
This process involves breast implant placement under the chest muscle. The technique reduces the risk of capsular contracture compared to sub-glandular placement.
Regular screening
Regular breast screening helps detect and treat many breast complications, including capsular contracture.
No-touch Breast Insertion Technique
Reducing contact of the breast implant with the external environment minimises the risk of bacterial contamination, reducing capsular contracture. Some tools surgeons use during surgical procedures that enhance the no-touch technique include the Keller Funnel and other techniques like double-implant loading, infusion containers, antibiotic irrigation, and reversed-glove sleeve.
Breast massage
Massaging the breast during the healing process may decrease the incidence of capsular contracture. However, a patient should perform breast massage with the help or authorisation of a surgeon.
Textured Breast Implants
Textured implants decrease the risk of capsular contracture by allowing the integration of the breast tissue with the implant. However, patients should avoid macro-textured silicone gel implants, which are banned in Australia due to the risk of BIA-ALCL (anaplastic large cell lymphoma).
Breast Implant Size
Large breast implants in patients with insufficient breast tissue may increase the risk of capsular contracture. The patient can also avoid capsular contracture by quitting smoking a few weeks before and after surgery and avoiding strenuous work after breast surgery. Moreover, the patient can consider waiting until the completion of radiation treatment after mastectomy before breast augmentation.
FAQs
Below are some of the common questions about capsular contracture.
Can Capsular Contracture Reoccur After Treatment?
Capsular contracture can reoccur after treatment. Treatment of capsular contracture doesn’t guarantee that the complication will not develop again.
How Long Does It Take for Capsular Contracture Occurrence After Breast Surgery?
Capsular contracture occurs any time, mostly during the healing process or within two years after breast surgery. However, there are incidences when the complication occurs years after surgery.
Can Capsular Contracture Affect Only One Breast?
Capsular contracture after breast augmentation surgery can affect one or both breasts.
Does the Type of Breast Implant Affect the Risk of Capsular Contracture?
No evidence shows the connection between capsular contracture and silicone or saline-filled breast implants. The risk of capsular contracture occurrence is equal in both types of breast implants.
Conclusion
Capsular contracture is the most common complication after breast implant surgery. The complication is associated with breast deformity, affecting breast aesthetics, and pain in severe cases. Most causes can be prevented or reduced, while some, like genetic predisposition, cannot. Capsular contracture occurs any time, mostly during the healing process or within two years after breast surgery.
References
- Noreña-Rengifo, B. D., Sanín-Ramírez, M. P., Adrada, B. E., Luengas, A. B., De Vega, V. M., Guirguis, M. S., & Saldarriaga-Uribe, C. (2022). MRI for Evaluation of Complications of Breast Augmentation. Radiographics, 42(4), 929–946.
- Brown, T. (2020). Plane change vs capsulotomy: A comparison of treatments for capsular contraction in breast augmentation using the subfascial plane. Aesthetic Plastic Surgery, 45(3), 845–850.
- Guimier, E., Carson, L., David, B., Lambert, J., Heery, E., & Malcolm, R. K. (2022). Pharmacological approaches for the prevention of breast implant capsular contracture. Journal of Surgical Research, 280, 129–150.
- Headon, H., Kasem, A., & Mokbel, K. (2015g). Capsular Contracture after Breast Augmentation: An Update for Clinical Practice. Archives of Plastic Surgery, 42(05), 532–543.
- De Kerckhove, M., & Iwahira, Y. (2020). Risk Factors for Capsular Contracture. Plastic and Reconstructive Surgery. Global Open, Publish Ahead of Print.
- Araco, A., Caruso, R., Araco, F., Overton, J., & Gravante, G. (2009). Capsular Contractures: A Systematic Review. Plastic and Reconstructive Surgery, 124(6), 1808–1819.
- Salibian, A. A., Frey, J. D., Bekisz, J. M., Choi, M., & Karp, N. S. (2019). Fat Grafting and Breast Augmentation. Plastic and Reconstructive Surgery. Global Open, 7(7), e2340.
- Swanson, E. (2016). Open Capsulotomy. Plastic and Reconstructive Surgery. Global Open, 4(10), e1096.
- Fosheim, K., Bojesen, S., Troestrup, H., & Lænkholm, A. V. (2022). Capsulectomy Can Successfully Treat Chronic Encapsulated Breast Seroma: A Case Report. Cureus.
- Zhu, L., Zhu, J., Qian, Y., & Jiang, H. (2021). Reduced capsular contracture with smooth and textured breast implants following submuscular mammoplasty: systematic literature review. Future Oncology.
- Morkuzu, S., Ozdemir, M., Leach, G. A., Kanapathy, M., Mosahebi, A., & Reid, C. M. (2022d). Keller Funnel Efficacy in “No Touch” Breast Augmentation and Reconstruction: A Systematic Review. Plastic and Reconstructive Surgery. Global Open, 10(11), e4676.
- Wong, C., Samuel, M., Tan, B., & Song, C. (2006). Capsular Contracture in Subglandular Breast Augmentation with Textured versus Smooth Breast Implants: A Systematic Review. Plastic and Reconstructive Surgery, 118(5), 1224–1236.
- Handel, N., Cordray, T., Gutierrez, J., & Jensen, J. (2006). A Long-Term Study of Outcomes, Complications, and Patient Satisfaction with Breast Implants. Plastic and Reconstructive Surgery, 117(3), 757–767.
- Steinbach, B. G., Hardt, N. S., Abbitt, P. L., Lanier, L. L., & Caffee, H. H. (1993b). Breast implants, common complications, and concurrent breast disease. Radiographics, 13(1), 95–118.